Korean 3D bioprinting specialist T&R Biofab has patented a way of creating human tissues that could one day be used to develop a heart disease treatment which doesn’t put patients through open surgery.
Utilizing T&R Biofab’s process, scientists have already proven it possible to create 100-micrometer cardiac spheroids, capable of regenerating damaged tissues upon transplantation. While the technology remains at a pre-clinical stage, the firm’s patent approval in Japan could now be significant, in that the only developer of something similar in the country, has reportedly licensed it out for $600 million.
Regenerative cardiac therapy
According to CDC heart disease data, cardiac illnesses are the leading cause of death in men and women across most racial and ethnic groups in the US. As such, the development of robust cardiac therapies is a matter of life and death for many Americans. Yet, despite the urgency surrounding the issue, the T&R Biofab scientists behind its spheroid research say that current treatments are “unrealistic.”
Due to the “limitations and drawbacks” associated with transplantation, as well as the installation of pumps into the ventricles of patients’ hearts, the scientists have therefore identified cell-based regenerative treatments as an alternative.
Generally speaking, such methods involve using cardiomyocytes (the cells that make a heart contract) derived from human pluripotent stem cells to develop transplantable tissues, with the likes of Matricelf taking a similar path towards creating 3D bioprinted neural implants last year.
In the field of cardiac 3D bioprinting research, scientists also continue to make rapid advances, and a team at Harvard University recently found they were able to produce functional multi-layered heart tissues. However, as the T&R Biofab researchers point out in their spheroid paper, the heterogeneity of stem cells remains an issue that makes them extremely difficult to store and use long-term.
“Major issues, including the heterogeneity of human pluripotent stem cells, may cause tumorigenicity and arrhythmia, and affect their long-term storage, causing their poor survival, retention, and engraftment in-vivo following implantation into diseased hearts,” said the T&R Biofab-led team in their paper. “These issues must be resolved before pursuing clinical application.”
Improving cardiac tissue viability
One of the early breakthroughs in the scientists’ research was their discovery that cluster of differentiation 71 (CD71) surface proteins are key to creating tissues formed of homogenous stem cells. While generally used inside the human body for delivering iron, the researchers found that CD71 also plays an important role in the heart, and when added to tissues, it can trigger microfibrillar cell growth.
Having come up with a way of improving cell viability, the team then turned to developing a means of better preserving tissues during storage, something that could be key to their future clinical usage. To achieve this, the team came up with the idea of cardiac spheroids, essentially groups of human pluripotent stem cells, which, when packed together, are capable of surviving for longer periods.
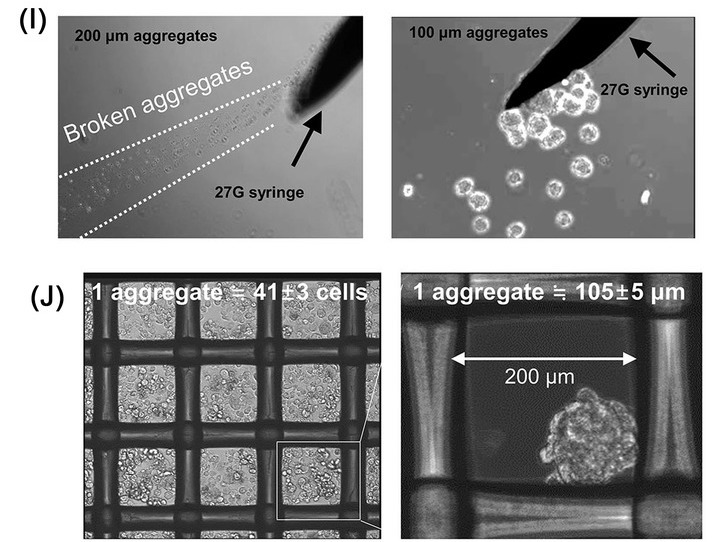
As a means of testing the long-term viability of these structures, the scientists later created prototypes before freezing them with liquid nitrogen. When defrosted six months later, it was discovered each of the spheroids was uniform in size, and that 80% of the tissues’ cells were still viable. Over shorter 7-day trials, samples also lasted demonstrably longer than single-cells or larger aggregate clusters.
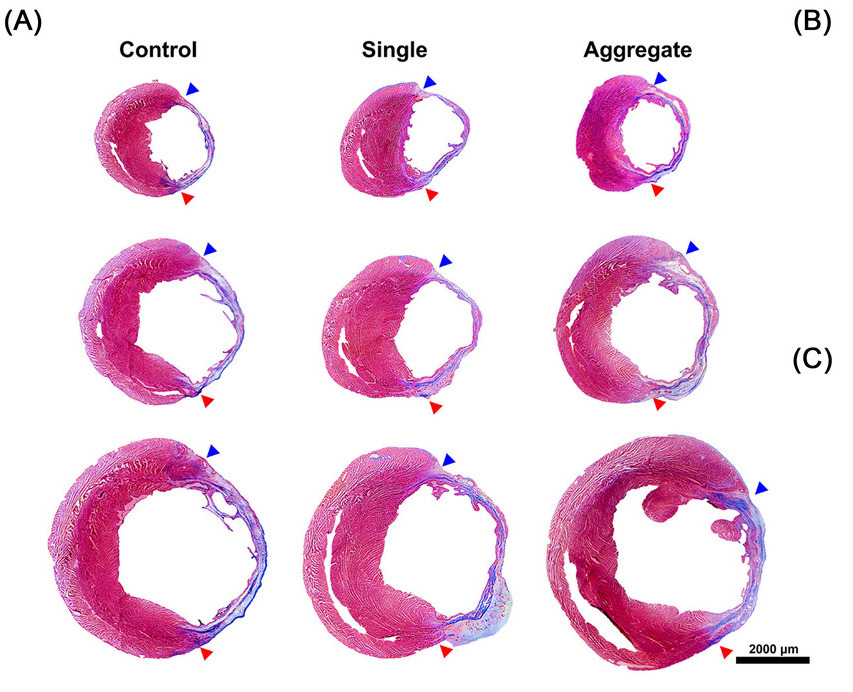
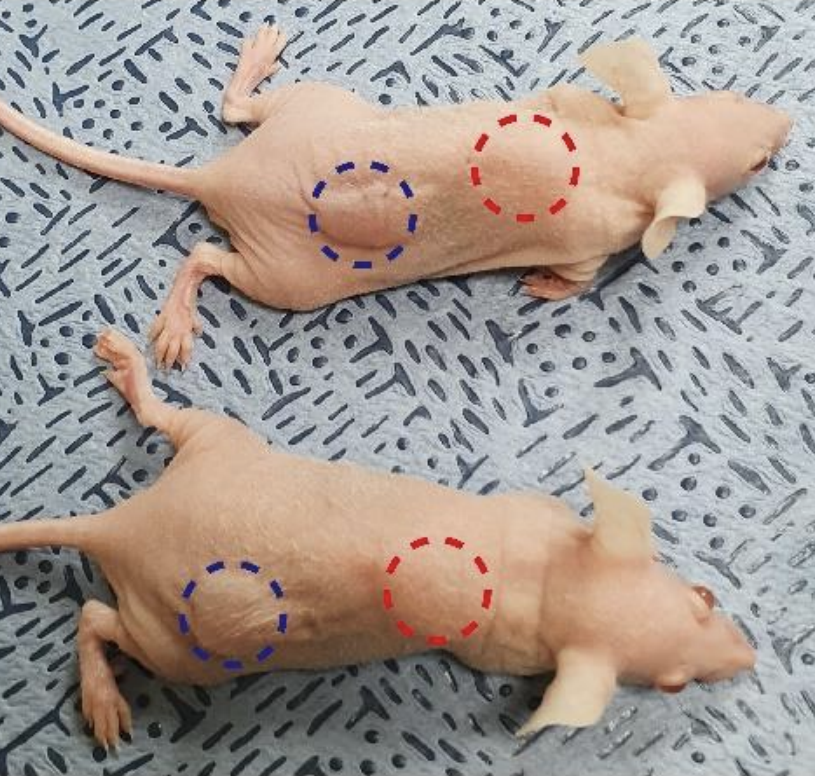
Once they’d proven the efficacy of their overall approach, the last stage of the team’s study saw them test their spheroids, by implanting them into rats entering cardiac arrest. Those treated with the scientists’ tissues were found to exhibit higher levels of cardiac function than those treated with regular stem cells, and following removal, the spheroids ultimately showed excellent engraftment and stability.
“The approach described in this study is simple and effective for the production of readily available human pluripotent stem cells in clinical settings,” the scientists concluded in their paper. “The microcardiac spheroids established in this study can be preserved and stored; they exhibit superior viability under hypoxic conditions and in-vivo. [However], despite several meaningful results, future studies examining more sophisticated implantation methods, such as the 27G NOGA catheter system and applicability to large animals, are considered limitations of this study.”
Although viable 3D bioprinted soft tissue transplants remain a long way from reality, the technology continues to make progress in lab settings. T&R Biofab itself found that it was able to implant 3D bioprinted liver tissues into animal test subjects last year, in a project that saw its scientists replicate the ‘lobules’ of the human liver.
More recently, researchers at the University of California, Berkeley have also uncovered a way of ensuring the viability of 3D bioprinted structures by freezing them. The team’s novel approach to ‘3D Cryoprinting’ allows for the cross-linking of cells layer-by-layer, in a way that yields self-supporting structures with potential in regenerative medicine R&D.
The research behind T&R Biofab’s microcardiac spheroids technology is detailed in the paper titled “Effect and application of cryopreserved three-dimensional microcardiac spheroids in myocardial infarction therapy.”
The study was co-authored by Soon-Jung Park, Hyeok Kim, Sunghun Lee, Jongsoo Kim,Taek-Hee Jung, Seong Woo Choi, Bong-Woo Park, Sun-Woong Kang, David A. Elliott, Edouard G. Stanley ,Andrew G. Elefanty, Kiwon Ban, Hun-Jun Park and Sung-Hwan Moon.
As you’d expect from such a large team, they hailed from multiple organizations, including T&R Biofab’s Research Institute, the Catholic University of Korea, the City University of Hong Kong, Konkuk University, Seoul National University, the Korean Institute of Toxicology, and Monash University.
To stay up to date with the latest 3D printing news, don’t forget to subscribe to the 3D Printing Industry newsletter or follow us on Twitter or liking our page on Facebook.
For a deeper dive into additive manufacturing, you can now subscribe to our Youtube channel, featuring discussion, debriefs, and shots of 3D printing in-action.
Are you looking for a job in the additive manufacturing industry? Visit 3D Printing Jobs for a selection of roles in the industry.
Featured image shows cardiac fibrosis occurring in spheroid samples after 8 weeks. Image via T&R Biofab.



