Researchers from the University of Minnesota (UMN) have worked with medical technology firm Medtronic to develop realistic customizable 3D printed aortic models.
Using tailor-made silicone-based polymeric inks, the UMN team fabricated lifelike duplicates of a human aortic root, the vascular section which is attached closest to the heart. The patient-specific replicas could enable surgeons to better prepare for minimally invasive procedures, improving surgical outcomes for cardiovascular patients in the process.
“Physicians can actually test and try the valve implants before the procedure,” explained Michael McAlpine, lead researcher on the study. “Our goal with these 3D printed models is to reduce medical risks and complications by providing patient-specific tools to help doctors understand the exact anatomical structure and mechanical properties of the specific patient’s heart.”
The hidden dangers of cardiovascular surgeries
As advances in medicinal technology continue to raise life expectancies around the world, maintaining the health of an increasingly aging population has become a pressing issue. Elderly people are particularly vulnerable to cardiovascular diseases, and the common Noncongenital Aortic Stenosis (AS) condition affects 2.7 million people aged over 75 in North America alone.
AS causes the aortic valve to narrow, leading to restricted blood flow from the left ventricle to the aorta, and ultimately to ventricular dysfunction. Given the advanced age of patients that tend to suffer from AS, it is often deemed too risky for many AS patients to receive surgical valve replacement via open heart surgery.
Transcatheter aortic valve replacement (TAVR) offers a minimally-invasive alternative method of aortic treatment. Using a catheter delivery system, a bioprosthetic valve can be implanted into the biological valve, preventing blockages from taking place. Still, like any surgical procedure, TAVR is subject to potential complications, and disturbances triggered by interactions between the prosthetic and the patient’s anatomy can cause leakages.
Paravalvular Leaks (PL) can be serious, and result in left bundle branch blockages or atrioventricular obstruction, leaving the patient needing a permanent pacemaker to live. PLs aren’t necessarily caused by surgical errors though, and a patient’s anatomy and the prosthetic valve’s dimensions can also contribute to post-TAVR complications. As a result, creating implants that are custom-made for individual patients, is vital to surgical success.
The UMN team’s 3D printed aortic valve models
Although 3D printing offers the potential for heart models to be created in a way that precisely matches the biological original, previously printed aortic devices have been designed for post-operative use. As a result, existing heart root replicas have had no impact on the test patient’s chances of survival. Other duplicates have been printed for pre-operative applications, but comprise of rubber-like thermoplastics that don’t attempt to mimic the appearance of the genuine article.
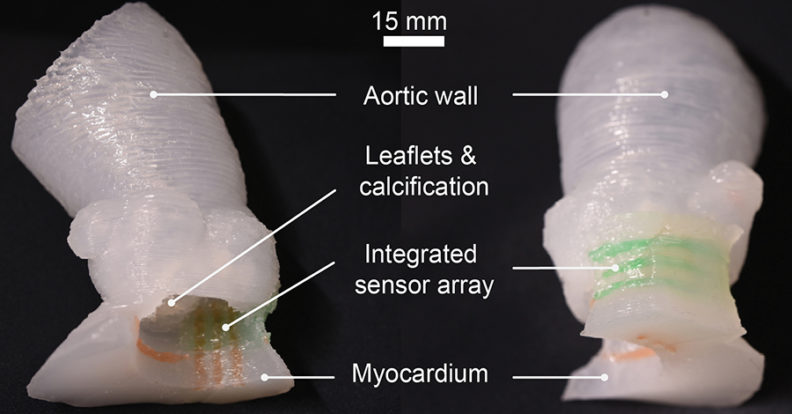
By contrast, the UMN researchers developed lifelike patient-specific models, featuring integrated sensors, which could allow doctors to mitigate the risks of disturbances during TAVR. The fabricated devices were also created using three different materials, with one for each of the aorta, myocardium and calcified regions.
To create a 3D model as a basis for their replica aortic implants, the research team carried out CT scans of a test patient’s cardiac anatomy. The aortic models, consisting of the aortic wall, a portion of the myocardium, leaflets, and calcifications, were 3D printed simultaneously using customized silicone-based polymeric inks. Crucially, the properties of the polymeric material could be adapted to match those of the patient, minimising any potential risk of complications.
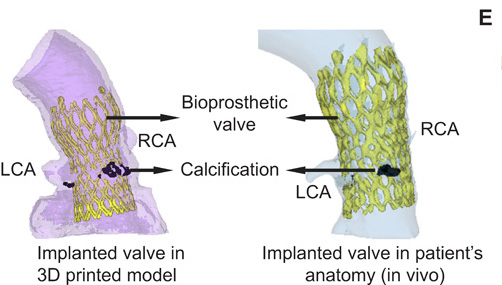
In order to assess the anatomic accuracy of their 3D printed models, the researchers CT scanned their replicas, and compared them to the scans of the original patient’s anatomy. Results showed that the team’s 3D printed replica was accurate to within 0.3mm across the implant, with peaks of 0 mm. In order to evaluate the pressure-sensing abilities of their device, the UMN team later implanted a 29-mm valve into the test patient with three different heights.
Mapping the pressure distribution in each case revealed pressure values of 234, 486, and 404 kPa had been generated during surgery. According to separate research carried out using Medtronic implants, contact pressures from 0.43 to 0.7 MPa can cause surgical disturbances, placing the team’s models at the lower end of the spectrum. As a result, the researchers had successfully identified a causal link between patients’ features and the risk of complications.
The UMN research team concluded that the sensor array built into their additive implants has the potential to be combined with many existing clinical practices. Additionally, the customizable nature of the team’s devices could enable doctors to minimize the risk to cardiovascular patients through a more thorough surgical pre-planning process.
A brief history of additive aortic models
A number of universities have also developed 3D printed aortic models in recent years, with the overall ambition of improving the surgical outcomes of aortic surgeries.
An associate professor of radiology and cardiology at the University of Kentucky (UK) College of Medicine, is 3D printing custom heart models to aid physicians and their patients. The low-cost fabricated aortas cost just $5, and are being produced as an accurate, pre-surgical tool to enable precise fittings of heart-assisting implants.
Scientists from ETH Zürich and medical device manufacturer Strait Access Technologies (SAT) are also developing 3D printed heart valves from silicone. By combining CT scanning with computer simulation, the team have been able to calculate the forces acting on the artificial valve implant and its potential deformation.
Researchers from the Wyss Institute at Harvard University, have created a 3D printing workflow to predict the performance of artificial heart valves during heart operations. In a “try before your buy” approach, the team’s software simulates a valve’s reaction with a patient’s native tissue, providing accurate medical models that are specific to each individual patient.
The researchers’ findings are detailed in their paper titled “3D printed patient-specific aortic root models with internal sensors for minimally invasive applications,” which was published in the Science Advances journal. The report was co-authored by Ghazaleh Haghiashtiani, Kaiyan Qiu, Jorge D. Zhingre Sanchez, Zachary J. Fuenning, Priya Nair, Sarah E. Ahlberg, Paul A. Iaizzo and Michael C. McAlpine.
Nominations for the 2020 3D Printing Industry Awards are still open, let us know who is leading the industry now.
The fourth edition of the 3D Printing Industry Awards Trophy Design Competition is now underway. Enter your design for the chance to win a CraftBot Flow 3D printer.
To stay up to date with the latest 3D printing news, don’t forget to subscribe to the 3D Printing Industry newsletter or follow us on Twitter or liking our page on Facebook.
Are you looking for a job in the additive manufacturing industry? Visit 3D Printing Jobs for a selection of roles in the industry.
Featured image shows a 3D scan of the UMN team’s 3D printed aortic valve. Image via UMN.



