The 2021 3D Printing Industry Awards shortlists are open for voting, have your say now.
A team of scientists from the Israel Institute of Technology (Technion) have used 3D printing to form a network of blood vessels capable of supplying blood to implanted tissue.
Led by Technion Professor Shulamit Levenberg, the researchers 3D printed a tissue flap with a blood vessel network that, reportedly for the first time, contains a functional combination of both big and small blood vessels.
The development could potentially remove the intermediary step of first transplanting a tissue into a healthy limb of a patient to enable it to be permeated by the body’s blood vessels, before transplanting it into the affected area. 3D printing the blood vessels also enables greater customization for patients and could help to reduce the risk of implant rejection.
3D printing blood vessel networks
Blood vessel networks are vital for the transportation of oxygen and nutrients to the body’s tissues and organs. Transplanted tissues need the same blood vessel support in order to be accepted into the body and function successfully.
Backed by the European Research Council (ERC) under the EU’s Horizon 2020 Research and Innovation Programme, Dr Ariel Alejandro Szklanny of Levenberg’s Stem Cell and Tissue Engineering Laboratory at Technion sought to create a hierarchical blood vessel network for transplanted tissues leveraging 3D printing.
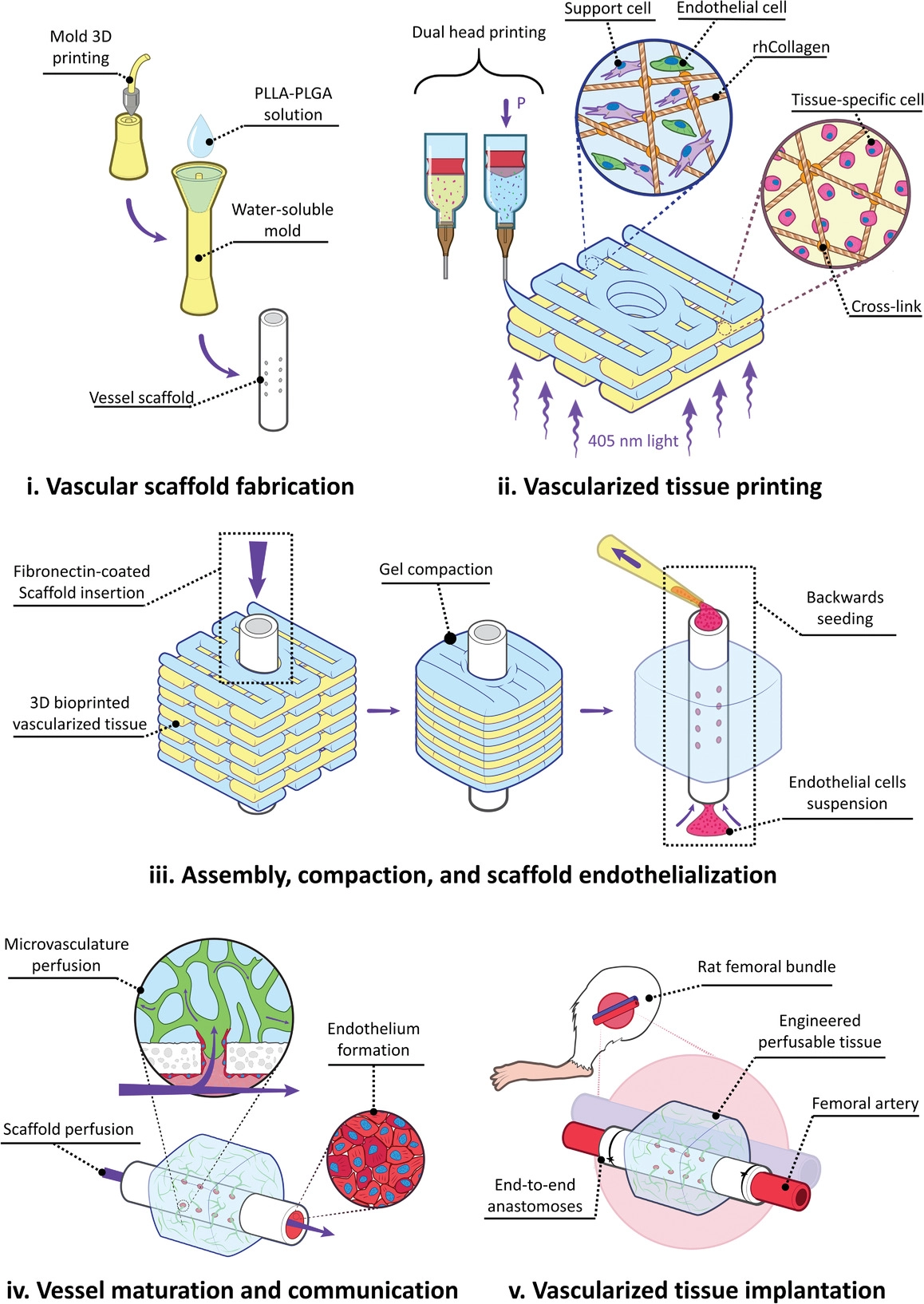
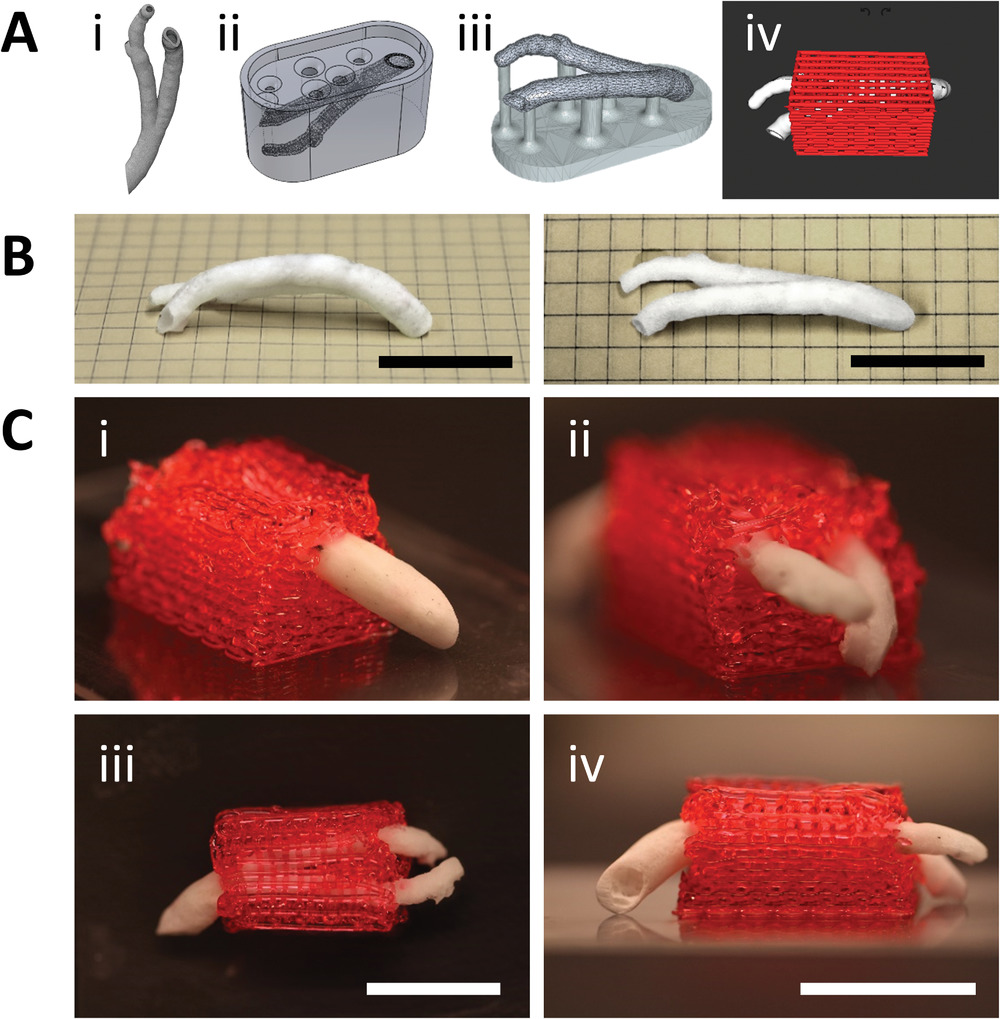
He began by 3D printing a polymeric scaffold that mimicked the size and shape of a large blood vessel. The scaffold was printed in the form of a hollow tube with side openings to allow the attachment of smaller blood vessels. In contrast to previous studies where collagen from animals has been used to form scaffolds, Szklanny used human collagen engineered by Israeli bioprinting firm Collplant which was derived from tobacco plants.
Once the scaffold had been created, tissue was 3D printed and assembled around it using another collagen-based bioink, and a network of tiny blood vessels formed within. The large blood vessel scaffold was then covered with endothelial cells, which make up the inner layer of blood vessels in the body.
The structure was incubated for one week, by which time the large scaffold had created functional connections with the smaller bioprinted vessels in the surrounding tissue to mimic the hierarchical structure of a human blood vessel network.
Improving tissue transplantation
To test the functional capabilities of the 3D printed blood vessel network, the Technion team transplanted the tissue structure into a rat, attaching it to the animal’s femoral artery. Blood was able to successfully flow through the transplanted tissue via the blood vessel network, without experiencing leaks.
According to the Technion team, the study constitutes an “important step” towards personalized medicines and demonstrates the viability of 3D bioprinting. The technology enables large blood vessels of the exact size and shape desired to be 3D printed and assembled together with the tissue that needs to be implanted.
Significantly, being able to implant a tissue with its own blood vessel network could eliminate the need to implant tissues into a healthy part of the body first so that it can be permeated by the body’s own blood vessels, before transplanting it again in the affected area. The fact that such tissue can be formed using a patient’s own cells could also substantially reduce, and even eliminate, the risk of the body rejecting the implant.
Going forwards, the Technion team will continue to assess the scalability and translatability of their approach by adapting the 3D printed blood vessel networks to be implanted in larger animals, such as pigs. The team believe their technique could cement a new path toward fully lab-grown patient-specific tissues that are suitable for transplantation.
Further information on the study can be found in the paper titled: “3D bioprinting of engineered tissue flaps with hierarchical vessel networks (VesselNet) for direct host-to-implant perfusion,” published in the Advanced Materials journal. The study was co-authored by A. Szklanny, M. Machour, I. Redenski, V. Chochola, I. Goldfracht, B. Kaplan, M. Epshtein, H. Yameen, U. Merdler, A. Feinberg, D. Seliktar, N. Korin, J. Jaroš, and S. Levenberg.
Blood vessel 3D printing
Additive manufacturing techniques have been leveraged for the creation of blood vessel mimicking structures in the past, with researchers seeking to provide alternative methods for drug development, eliminating human and animal testing, and disease treatments.
Back in 2018, researchers from CU Boulder developed a 3D printing method that used controlled oxygen inhibition to imitate the structure and geometry of blood vessels. The aim of the study was to create microstructures that could be customized for disease modeling.
Around the same time, bioengineers from the University of California San Diego developed a 3D bioprinting method to produce lifelike organ tissue models containing blood vessel networks. The networks were able to keep a breast cancer tumor alive outside the body, as well as forming a model of a vascularized human gut.
More recently, researchers have used a modified 3D cell printing technique to produce a biomimetic blood vessel that was successfully implanted into a living rat, and a team from Texas A&M University 3D bioprinted a highly realistic blood vessel model made of a new nanoengineered hydrogel bioink. The hydrogel closely mimics the natural vascular function and disease response of a real blood cell, and could potentially pave the way for advanced cardiovascular drug development.
Subscribe to the 3D Printing Industry newsletter for the latest news in additive manufacturing. You can also stay connected by following us on Twitter and liking us on Facebook.
Looking for a career in additive manufacturing? Visit 3D Printing Jobs for a selection of roles in the industry.
Subscribe to our YouTube channel for the latest 3D printing video shorts, reviews and webinar replays.
Featured image shows coronary VascFold fabrication and integration with a 3D printed surrounding hydrogel structure. Image via Advanced Materials.


