At Charité–Universitätsmedizin Berlin, “Europe’s largest University clinic,” researchers are working to prove that, in specific cases, 3D printed titanium-mesh scaffolds offer a better alternative to conventional bone-grafting techniques using a patient’s own bone.
The treatment is believed to be particularly effective when treating large bone defects caused by significant trauma to the limbs. In addition to unparalleled strength, 3D printed titanium implants can be designed to fit any injury. Made with complex inner geometries, in a number of cases, such implants have proved more effective at encouraging in-growth of bone and vascular structure essential to a patient’s full recovery.
In order to prove their hypothesis, Charité researchers successfully conducted a large animal study using 3D printed titanium-mesh scaffolds with a pool of 27 sheep. The study then moved to a pre-clinical trial of 19 human patients. Science Translational Medicine has published the results.
Mechanically and biologically optimised meshes
The titanium-mesh scaffolds in the Charité study were 3D printed by DePuy Synthes using a metal laser sintering process.
The implants were designed with a honeycomb-like structure. By altering the strut diameter of the honeycomb, researchers could create a stiffer implant and maximize support.
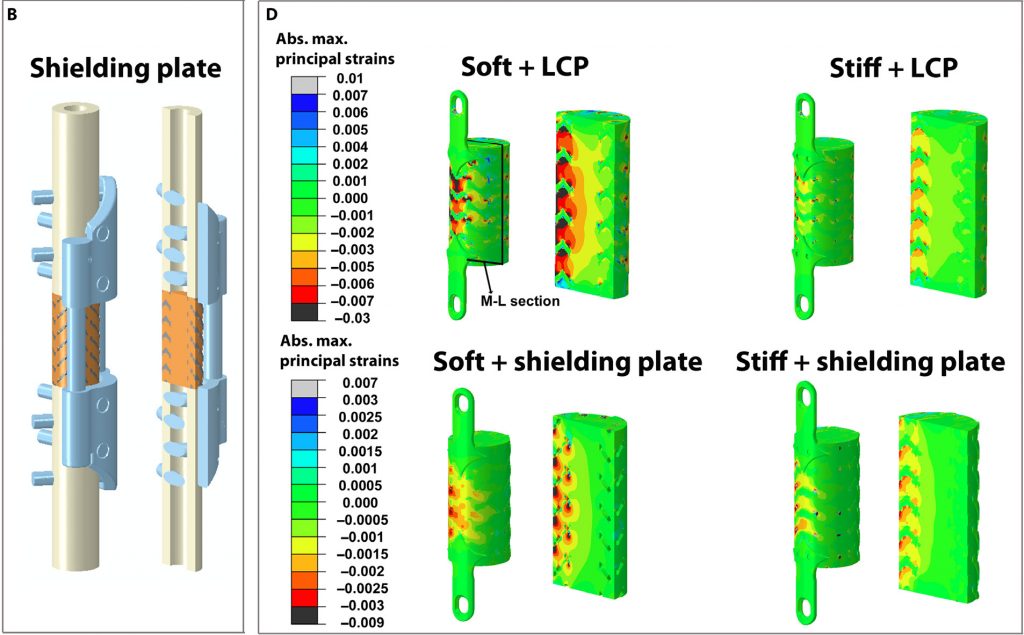
The team also experimented with two reinforcement mechanisms for the implants; a shielding plate, and a locking compression plate (LCP), as shown in the diagram below.
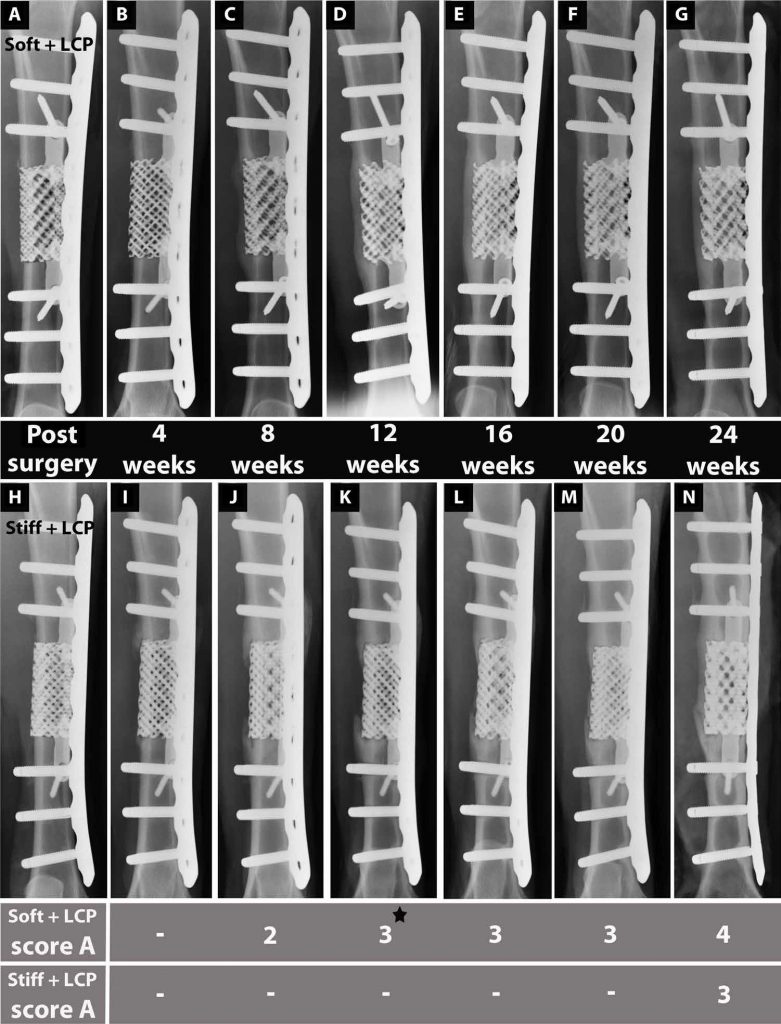
24 weeks post surgery, the titanium-mesh scaffolds proved to “enhance bone regeneration” when implanted in sheep.
As a result, the decision was made to move to a pre-clinical trail with human patients.
Trial and error
Each of the pre-clinical implants were made to patient-specific requirements. Perhaps critically though, the implants were not mechanobiologically optimized in the same way they were with sheep.
Of the 19 diverse patients selected for the study, two returned with negative bone in-growth on the implants. Nevertheless, the “study supports the hypothesis that endogenous bone defect regeneration within 3D Ti-mesh scaffolds can be promoted by minimizing the scaffold mechanical stiffness.” And bone regeneration through mechanobiological optimization was enhanced in the treatment of sheep.
Full details can be found online in the paper“Mechanobiologically optimized 3D titanium-mesh scaffolds enhance bone regeneration in critical segmental defects in sheep.”
This research was co-authored by Anne-Marie Pobloth, Sara Checa, Hajar Razi, Ansgar Petersen, James C. Weaver, Katharina Schmidt-Bleek, Markus Windolf, Andras Á. Tatai, Claudia P. Roth, Klaus-Dieter Schaser, Georg N. Duda, and Philipp Schwabe.
The work was completed by Charité–Universitätsmedizin Berlin in collaboration with the Max Planck Institute of Colloids and Interfaces, Wyss Institute, AO Research Institute Davos and Technical University Dresden.
Nominate the best research teams of 2017 in the second annual 3D Printing Industry Awards here.
Subscribe to the 3D Printing Industry newsletter, follow us on Twitter, and like us on Facebook here.
Featured image shows evidence of Charité’s improved 3D titanium implants at various stages post-surgery. Image via Science Translational Medicine



