The 2021 3D Printing Industry Awards shortlists are open for voting, have your say now.
Scientists from the Nakayama Lab at Saga University and Kyoto University in Japan have fabricated 3D printed cartilage constructs from stem cells which could potentially be used to repair large cartilage defects in patients.
Using human induced pluripotent stem cells (iPSCs), the researchers created the cartilage structures using a scaffold-free Kenzan bioprinting process, where the only support structure of the bioink is a microneedle matrix.
The technique reportedly enabled the scientists to overcome the limitations of scaffold-based tissue engineering methods for creating cartilage-like structures, such as poor cytocompatibility and toxicity, while solving the problem of bacterial infection and some risks associated with replacement surgery that conventional joint prostheses have.
The aim of the study is to treat conditions such as arthritis in athletes who do not want to undergo treatment with artificial joints made of metal and plastic.
Improving arthritis treatment
Articular cartilage is a load-bearing connective tissue that covers the ends of bones to prevent friction and protect joints. Cartilage damage can occur as a result of disease, trauma, and degenerative conditions such as osteoarthritis, one of the leading causes of joint pain and immobility.
Over 300 million people worldwide suffer from osteoarthritis, causing a huge clinical and economic burden. Current surgical treatments, such as microfractures and implants, typically only focus on focal defects and do not generate long-lasting functional cartilage. Total joint replacement is also the only treatment for end-stage osteoarthritis, with implants lacking durability over extended periods of time and potentially leading to bone shortening and other complications.
Tissue engineering is an alternative to total joint replacement for cartilage repair and joint preservation, however the method is limited by a lack of functional cell types and biomaterials. Chondrocytes and mesenchymal stem cells (MSCs) are currently considered the most promising sources of cells for regeneration therapy, although they can be hampered by donor age, density, activity, cell phenotype and other factors.
iPSCs are an alternative cell source that show promise in overcoming some of these limitations, due to their self-renewal potential to provide an almost unlimited number of cells with pluripotent capabilities – the ability to differentiate into many different cell types. As such, iPSCs were chosen as the basis of the scientists’ cartilage structures.
3D printing cartilage
Present tissue engineering technologies for cartilage regeneration can largely be separated into scaffold-based and scaffold-free methods, with 3D printing having been leveraged for multiple research projects in this area in the past.
For instance, scientists from the Chalmers University of Technology have previously demonstrated cartilage tissue engineering to treat osteoarthritis using 3D bioprinting, and microbiologists at Central Queensland University have explored a combination of crocodile protein and 3D bioprinting to repair joint damage. Elsewhere, Penn State researchers have developed a novel 3D printing method to create cartilage tissue building blocks with micropores that allow nutrient and oxygen diffusion.
More recently, researchers at the University of Alberta have developed a method of 3D bioprinting customized nasal cartilage for cancer patients living with post-operative facial disfiguration, and Swansea University is 3D printing cartilage tissue scaffolds for scar-free ear and nose transplants in partnership with the Scar Free Foundation.
One high-profile initiative that is currently making headway in this area is the EU-backed TRIANKLE project, which is seeking to develop 3D bioprinted cell-restoring ankle implants. Last year, the project received the backing of Spanish football club FC Barcelona’s R&D lab, which has agreed to test the collagen-based cell graft transplants on its amateur squad with a view to eventually prepare them for future commercial release.
3D printing cartilage protheses with iPSCs
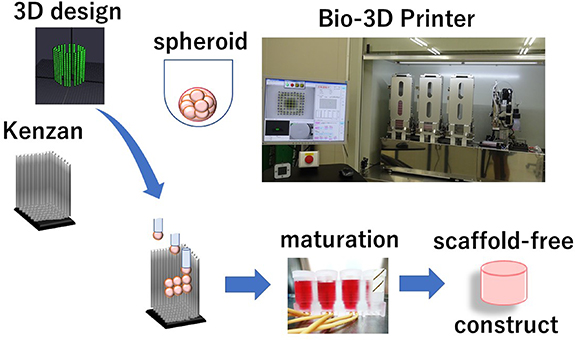
The aim of the Japanese scientists’ current study was to leverage a 3D bioprinter to engineer a scaffold-free cartilage structure of anatomical size and shape. A Regenova Bio-3D printer from Cyfuse Biomedical was used for the study. The Regenova is a novel robotic system that facilitates the fabrication of 3D cellular structures by placing cellular spheroids in fine needle arrays, the Kenzan method, according to pre-designed 3D data.
The printer leveraged a 9 x 9 square Kenzan array consisting of 81 needles, a 26 x 26 square Kenzan array of 676 needles, and a 7 mm diameter round-type Kenzan array of 36 needles in a single row, in order to 3D print various sizes of cartilage protheses.
First, iPSCs were differentiated toward chondrocytes – metabolically active cells for cartilage formation – through MSC induction to form highly chondrogenic and potent iNCMSCs. The iNCMSCs were then optimized for the bioprinting process, after which a minimum maturation period was determined. Then, the various types of Kenzan listed above were deployed to fabricate larger cartilage constructs that were specifically shaped for irregular defects.
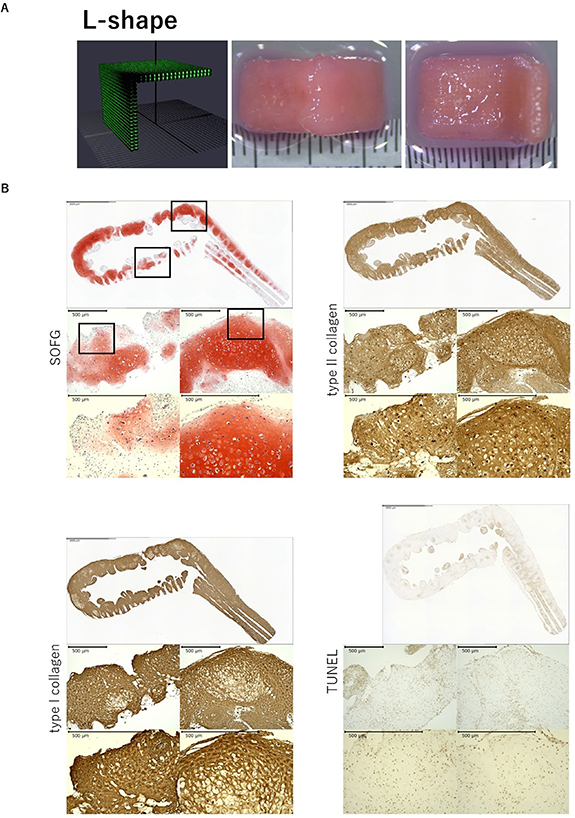
The first construct, which confirmed the method’s potential to sustain shape, was printed in an L-shape with a 90-degree angle. After removal from the Kenzan, the construct was able to maintain the applied design and withstand mechanical manipulation regardless of its 2 cm square total area.
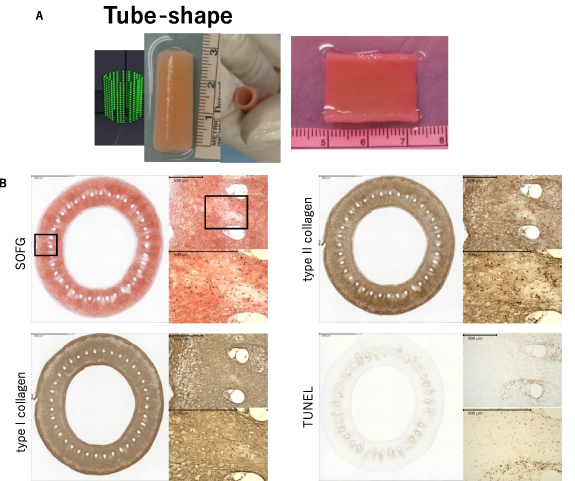
Applying the 7 mm round Kenzan, the scientists were able to increase the construct size up to 6 cm squared in a half-pipe-shaped structure which could be utilized to treat a wide, curved area such as the patellar surface.
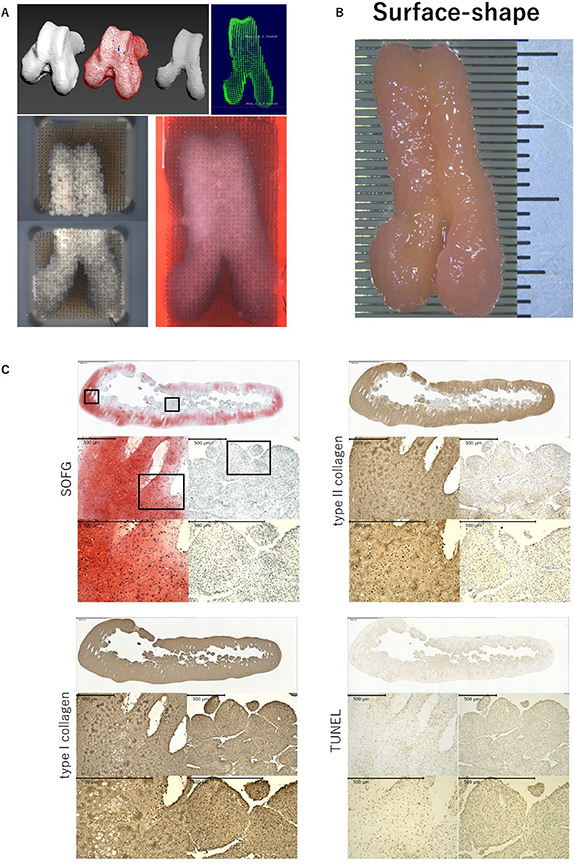
Through their approach, the scientists were able to successfully 3D print scaffold-free, self-sustainable cartilage constructs of a suitable size and shape for repairing larger cartilage defects. The constructs were also found to exhibit a strength almost equal to that of normal cartilage.
The durability of the scientists’ cell-based joint prosthesis will continue to be assessed in future studies, and it is hoped that it will solve the problem of bacterial infection and some risks associated with replacement surgery that conventional joint prostheses have.
However, they did note that while using iPSC-derived cells as a source material has many benefits, it remains extremely expensive. Therefore, they state that further optimization and improvement of the technology will be crucial before they can conduct even more time and money-consuming studies in vitro.
Further information on the study can be found in the paper titled: “Bio-3D printing iPSC-derived human chondrocytes for articular cartilage regeneration,” published in the Biofabrication journal. The study is co-authored by A. Nakamura, D. Murata, R. Fujimoto, S. Tamaki, S. Nagata, M. Ikeya, J. Toguchida, and K. Nakayama.
Subscribe to the 3D Printing Industry newsletter for the latest news in additive manufacturing. You can also stay connected by following us on Twitter and liking us on Facebook.
Looking for a career in additive manufacturing? Visit 3D Printing Jobs for a selection of roles in the industry.
Subscribe to our YouTube channel for the latest 3D printing video shorts, reviews and webinar replays.
Featured image shows schematic representation of the 3D printing process. Image via Biofabrication.



