Researchers from the Georgia Institute of Technology and Hanyang University, Korea, have developed the first aerosol jet printed (AJP) biosensor for wireless monitoring of blood flow.
In a study published in Advanced Science, the team have used a novel AJP technique to 3D print an implantable and stretchable electronic system. This maintains a circuit-free and low-profile design with enhanced readout distances, capable of monitoring blood flow in the brain for aneurysm treatments.
Implanted wireless monitoring devices
Wearable tech refers to smart electronic devices that can be worn or implanted in the body. 3D printing has enabled new wearable devices such as electronic second skins, and smart fabrics. Furthermore, in combination with soft materials, stretchable and flexible devices like biosensors have been developed.
The functionality of these sensors depends heavily on their wireless monitoring capabilities which is enabled by rigid circuitry. Nevertheless, according to the researchers, rigid circuitry leads to incompatibility with soft tissues or blood vessels.
“The rigid electronics based on metals and plastics have a huge risk of thrombosis and flow disruption in a highly contoured blood vessel for monitoring of hemodynamics [dynamics of blood flow],” the study states.
Fabricating implantable sensors with aerosol jet printing
To address the shortcomings of conventional fabrication techniques, AJP was introduced to produce wireless implantable sensors. This technology allows for faster and reliable fabrication and scalable manufacturing via direct printing, digital designing, and optimized control.
In this study, the researchers developed a novel AJP approach for developing wireless stretchable electronics. Their biosensor utilizes polyimide as the dielectric layer and as a bottom supporting layer for a direct integration with a soft elastomer. The process starts with high precision 3D printing of four aligned layers, with ink composed of biocompatible silver nanoparticles and mixed polyimide (PI).
A small amount of of soft elastomer then connects the sensor to a medical stent. This seamless integration process enables the sensor to conform to the stent with high flexibility and stretchability. The resulting low-profile device can be deployed through conventional catheter procedures.

Wireless monitoring of hemodynamics
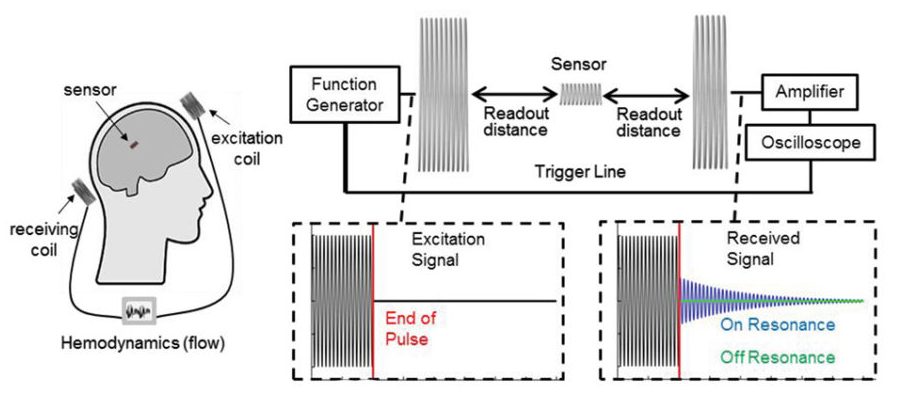
For wireless interrogation for implantation, the researchers utilized an inductive coupling method that offers a circuit-free design. This readout method applies inductive coupling principles between a sensor coil in a flow-diverter system and two external coils to record transient signals.
Following completion and optimization of the sensor system, in vivo experiments were carried out. Performance of optimal sensor coils in wireless detection of resonant frequencies through air, saline and meat were studied. The maximum readout distance through meat is found to be 6 cm, reaching the range for hemodynamics monitoring in the brain. The flow rate monitoring capabilities of the sensor was then tested in highly contoured and narrow human neurovascular models. The study adds:
“Collectively, this work shows the potential of the printed biosystem to offer a high throughput, additive manufacturing of stretchable electronics with advances toward batteryless, real-time wireless monitoring,”
The current limitation of this study is the integration of an implantable coil with the stent and sensor system to achieve a complete implantable package. Now, the team is developing methods for integration of an implantable, inductive coil with the existing stent and flow sensor.
Future work will involve hemocompatibility and biocompatibility tests of the sensor system. The effect of the properties of blood on the sensor and implantable coil, such as capacitive shorting between coil turns, will be further investigated.
“Fully Printed, Wireless, Stretchable Implantable Biosystem toward Batteryless, Real‐Time Monitoring of Cerebral Aneurysm Hemodynamics” is co-authored by Robert Herbert, Saswat Mishra, Hyo‐Ryoung Lim, Hyoungsuk Yoo, Woon‐Hong Yeo.
For more on additive manufacturing in academia, subscribe to our 3D Printing Industry Newsletter, follow us on Twitter, and like us on Facebook. Find talent for a project, or advance your career in 3D printing – join 3D Printing Jobs to apply and advertise.
Featured image shows the design of a highly stretchable sensor via finite element modeling and comparison with the fabricated sensor. Image via Georgia Institute of Technology/Advanced Science.



