In the 3D printing industry there are a few publicly shared case studies that were so successful that they are often used as examples for the future possibilities of 3D printing technologies. When it comes to polymer-based medical implants, the most important case is that where Dr. Glenn Green and Dr. Scott Hollister of the University of Michigan used 3D printing to produce a custom, bioresorbable tracheal splint for a child suffering from life-threatening tracheobronchomalacia (TBM).
This experimental operation completely changed the quality of life of the patient for the better and is now starting to become common practice, having saved the lives of four infants since 2013. Especially now that Materialise and University of Michigan signed a license agreement to produce the 3D Printed Tracheal Splints.
Arccording to the terms of the agreement, Materialise has entered into an exclusive licensing arrangement to take the splint through clinical trials, in order to ultimately offer the newly granted patent in the marketplace.“This agreement is a critical step in our goal to make this treatment readily available for other children who suffer from this debilitating condition,” Mott otolaryngologist Dr. Green said.
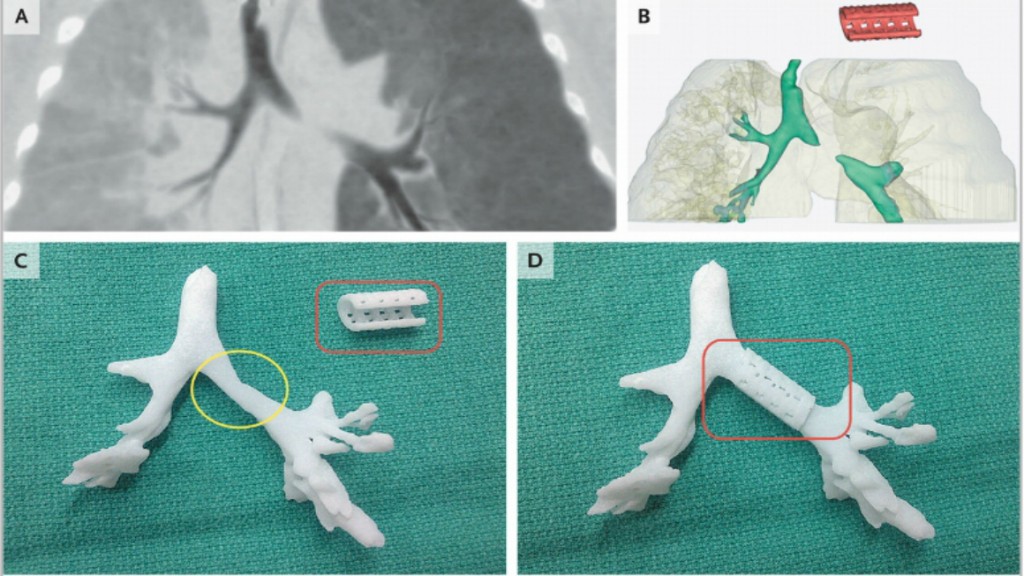
He and Dr. Scott Hollister used Materialise’s Mimics Innovation Suite to model and construct these splints using CT scans of patient anatomy. Dr Green was also present at Materialise’s latest MWC2015 conference in Brussels last spring, where he gave one of the most interesting presentations among dozens of top level talks on the past, present and future of 3D printed biomedical implants.
Materialise’s Mimics Innovation Suite was used to design the splint which is constructed from a bioresorbable technology platform licensed to Tissue Rigeneration Systems (TRS) by the University of Michigan in 2007. After several years refining fabrication methods, TRS received its first commercial product clearance from the FDA in 2013. The Materialise partnership is one of several co-development projects currently underway at TRS. Thanks to FDA approval for Expanded Access to an investigational medical device, the splints are now regularly used to treat TBM. “We are excited to have the opportunity to impact the lives of children affected with TBM through the production of the tracheal splint,” sad Jim Fitzsimmons, CEO of TRS.
“Here at Materialise, we strongly believe in the transformative power of great collaborations, such as the one we have enjoyed these past two years with Dr. Green, Dr. Hollister, and all others who have contributed to this live-saving application of 3D printing,” stated Bryan Crutchfield, Managing Director of Materialise USA. “This collaboration is proof that when the right skill sets and technologies are combined, solutions can be found for problems once thought impossible.”
About 1 in 2,200 babies are born with TBM, which causes the trachea to periodically collapse. The tracheal splint, developed to save the lives of these children, is made with a biopolymer called polycaprolactone, a biodegradable material that is gradually absorbed into the infant’s body tissue over time.
“It was the possibility to realize 3D-printing enabled medical applications that, in part, motivated me to start Materialise 25 years ago,” said Fried Vancraen,Founder and CEO of Materialise, “Today, we are proud to offer an entire range of software and services that can help universities, research centers, medical device companies, and hospitals develop solutions that result in a better and healthier world, such as the treatment developed for children diagnosed with TBM. It has been an honor to work with the team at University of Michigan, who are using our Mimics Innovation Suite to truly show the impact that patient-specific, 3D-printed solutions can have on the lives of individuals.”
The U-M team now hopes to next year open a clinical trial for 30 patients with similar conditions at C.S. Mott Children’s Hospital. “We have continued to evolve and automate the design process for the splints, allowing us to achieve in two days what used to take us up to five days to accomplish,” adds Scott Hollister, Ph.D., professor of biomedical Engineering and mechanical engineering. “I feel incredibly privileged to be building products that surgeons can use to save lives.” We also feel privileged to report on how 3D printing can truly and practically save and change lives.