The ability of 3D printing technology to revolutionize the way medicine operates continues to astound. Physicians can now use advances in 3D printing and materials to design devices to specifically fit the needs of their patients. Glenn Green, a pediatric ear, nose and throat specialist and researcher at the University of Michigan has had success with a new technique using 3D printers to create tiny, patient-specific splints that help give infants, born with defective airways, the ability to properly breathe.
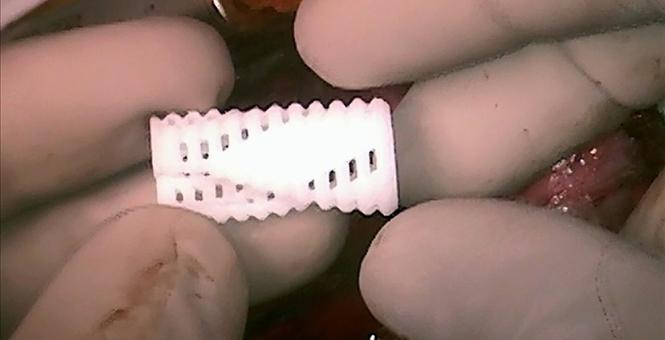
Unfortunately, about 1 in 2,000 babies is born with weakened bronchi, which can collapse and obstruct breathing. Luckily, most afflicted with the condition recover naturally by age 3, because their airways grow and become stronger. If the collapse and obstruction is severe enough, however, the condition can quickly become life-threatening. For this reason, Green and his colleagues invented a unique type of 3D printed airway splint, made with a special material that expands as the children grow and eventually dissolves when they are no longer necessary. Thus, Green and his team have added a fourth dimension to 3D printing: time.
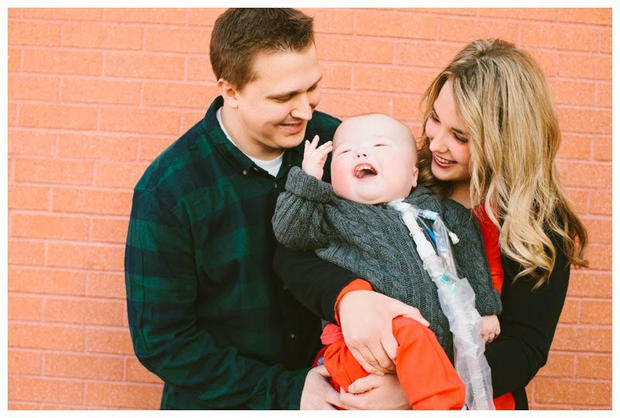
In 2013, Green’s team had initial success implementing this technique with Kaiba Gionfriddo, pictured above. Born with a weak bronchi, Kaiba, is now three years old and doing very well, breathing on his own. And the splint that is helping him breathe is dissolving at the rate that it was design to. Since its use with Kaiba, Green’s splints have gone on to potentially save the lives of two more of these fragile newborns.
At just 5-months-old, Ian Orbich’s breathing had stopped repeatedly, as he lay in the intensive care unit. Specialists in Pittsburgh ran out of options, but Ian’s mother, Meghan Orbich read a news article about the research in Michigan and contacted Green. Propping open Ian’s airways from the inside hadn’t worked optimally, so Green and biomedical engineer Scott Hollister designed an external splint to be stitched outside of his airways in order prop them open.
In order to create these splints, Green and Hollister took measurements from each patient’s CT scan and laser-sintered the personally-tailored tubes with openings down one side. Printed in just one day, the splints are made with a biodegradable plastic that begins to dissolve in about three years, the perfect amount of time to allow the airway passage to reinforce itself. After customizing the splint, the devices are then sterilized and prepared for surgery. Surgeons place the splint over the weakened airway and, as that airway doubles in size, they press on the splint and widen the opening. Surprisingly, the material cost of these patient-specific devices total only $10 a piece.
Eventually the low cost of printing the splint will hopefully make the surgery more affordable for many families. In addition to Kaiba and Ian, a third child, Garrett, has been in Green’s study at the University of Michigan. The condition of all three has improved dramatically and Kaiba and Ian have gone on to live ventilator-free lives. 17-month-old Ian is still on the ventilator, but his Mother is hopeful that the surgery will help him keep improving, saying, “He is doing amazing. It was a blessing.”
Time is a particularly important element when dealing with young children, and now that we have the materials to perform this kind of medical printing, there are many other exciting possibilities. Green is excited about his team’s accomplishments so far, “We are using laser light to transform dust into medical devices that change how the body develops. It is a concept that would have been inconceivable not too many years ago.”
Though Green and his team had to obtain special permission from the FDA to perform these surgeries, they hope that the clinical trials will prove that the 3D implant meets the same performance standards as regular implants. As they begin the clinical trial process, the team is working with the FDA to bring 3D printed splints to 30 other children.
Dr. Piers Barker, Duke University’s lead 3D printing researcher for pediatric cardiology, is enthusiastic about the future of the medical 3D printing field, “The promise of 3-D printing is you can really begin to personalize potentially almost every medical intervention. This approach to a structure that permits growth — this is the first time I’ve seen anything like this.”
We have seen a lot of innovation in the medical 3D printing field already, including replacement ears, custom artificial bones, and even models of organs that can help surgeons prepare for complicated surgical procedures. There are even those attempting to print human organs out of a blend of human cells and biodegradable scaffolding. These are all innovative ways to use 3D printing to revolutionize medical care, but there is something to be said for materials that expand and dissolve over time when working with the complex ecosystem of the human body. That is why the work of Green’s team at University of Michigan is so important. The 3D printed splints aid the body in forming an optimal breathing structure, instead of just replacing what doesn’t work.