Researchers from the Queensland University of Technology have released a study that challenges the Fused Deposition Modelling (FDM) 3D printing process behind the production of anatomical medical reconstructions.
3D printed models can be important tools for doctors, in diagnosing and treating patients, or educating and training future surgeons. In addition, medical models often serve as a more affordable and attainable alternative to using cadavers. Even so, inaccuracies and defects in these replicas, can potentially cause harm to patients through suboptimal treatment planning, and it’s vital that the process is fully-optimized as a result.

Additive manufactured medical models
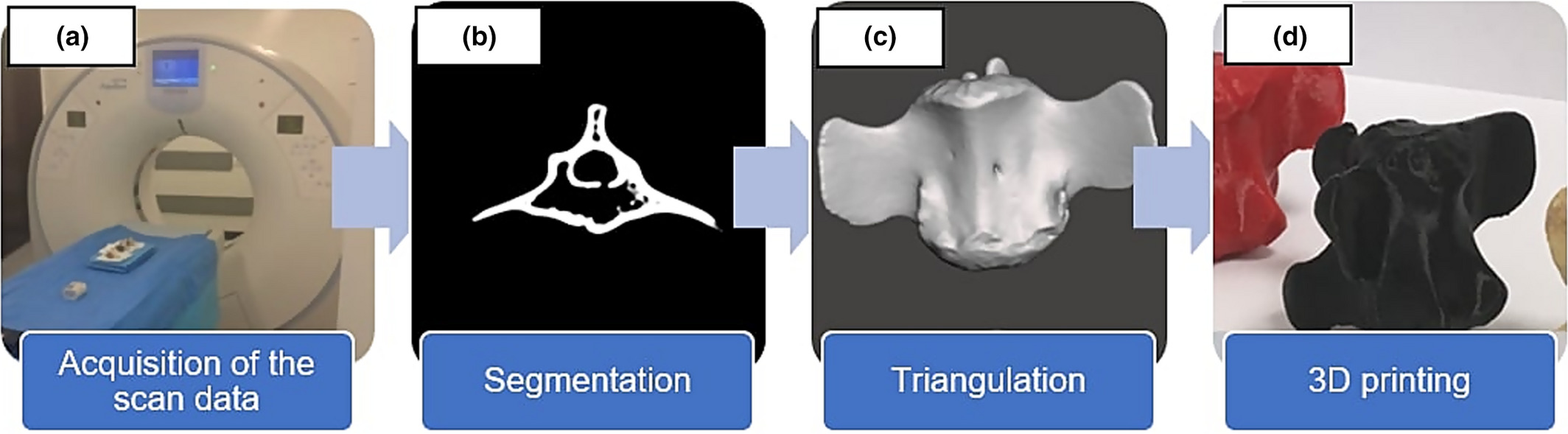
The FDM 3D printing process is well-suited to the production of medical devices, due to its size, cost and accessibility benefits. Nonetheless, it does have known drawbacks such as its inability to print features less than 0.3 mm in any dimension accurately, due to nozzle width limitations. CT scanners are often used to produce 3D visualizations of patient anatomies for 3D printing later in the process, and are considered to be the gold standard in 3D scanning according to the researchers. CT scans not only provide optimal hard tissue contrast and spatial resolution, but allow for the segmentation of anatomy, so that scan intensity automatically adjusts depending on the density of the tissue being replicated.
CT technology has not been perfected by any means though. In a single-detector CT scanner, the slice width is limited by detector size and the collimation of the x-ray beam along the z-axis. This could have a direct impact on 3D models created from an imaging data set, as higher slice widths result in lower image resolution and anatomical detail. Combining data from several detector elements can remedy this, by reconstructing images at a range of slice widths from the within the same scan, but with improved visualization. This can be achieved by decreasing slice reconstruction interval (SRI), which represents the distance between the centre of adjacent slices in scan data, but often produces less data.
Having identified a lack of research on the influence of SRI settings on the production of 3D printed anatomical models, the researchers aimed to determine if changing the slice reconstruction intervals in CT scan data, could improve the spatial replication accuracy. For the research team, determining if these settings produced accurate results, could be essential to producing accurate replicas, and reducing complications resulting from surgery.
The researchers’ findings on SRI
In order to test and determine the optimum SRI settings, three bovine coccygeal vertebrae and a European Forearm Phantom quality assurance device, were scanned using a 16 slice CT scanner. The specimens were positioned in line and imaged separately, in accordance with parameters commonly used in clinical practice, with the minimal slice width possible to maintain maximal resolution.
Data collected via the scans was transformed into a Digital Imaging and Communications in Medicine (DICOM) file of each original specimen, and a segmented model was created for each file. These replicas were then manufactured using a Malyan M200 3D printer, and once support structures were removed, measurements were taken of their anatomical features. The absolute error levels were summarily calculated as the absolute difference in millimeters between each original specimen measurement, and the corresponding 3D printed model.
Results showed that the 3D printing process had produced highly-realistic 3D replicas which were suitable for measurement and analysis. Absolute errors ranged from 0 to 1.91 mm, and increasing the SRI was shown to raise the mean absolute error between comparative measurements. Decreasing the SRI meanwhile, acted to reduce the mean absolute error between comparative measurements of paired models, but this was not the case all of the time, and the size of the data set produced means that this can make it a lengthy process.
In conclusion, the researchers found that reducing the SRI below the primary limiting factors, does not necessarily improve accuracy, and as a result, the added file size and processing time does not appear to be warranted. On the other hand, using an SRI significantly greater than the primary limiting factor potentially results in a loss of accuracy. By setting parameters similar to the primary limiting factor of acquisition slice width, was found to optimise the replication accuracy of the model, while minimising the size of the data and time investment.
The research team successfully demonstrated that changing the SRI influences the spatial replication accuracy of anatomical models, and predicted that their findings could reduce the risk of negative clinical impacts from inaccurate models in surgical applications.
3D printing and anatomical models
Additive manufacturing has been used to produce anatomically correct models of various parts of the human body.
In February 2020 for instance, a 3D printed tumour model designed by 3D LifePrints, a UK-based medical technology company, aided surgeons in the removal of a cancerous mass in a six-year-old girl. Additive manufacturing was utilized in order to establish the optimal approach for extracting 90% of the malignancy.
Researchers from the University of Kentucky (UK) College of Medicine, additive manufactured custom heart models to aid physicians and their patients in July 2019. The 3D printed hearts, costing $5, were produced as a pre-surgical tool to enable precise fittings of heart assisting implants.
Using a 3D printed model, French surgeons performed the world’s first robot-guided minimally invasive surgery on a scoliosis-affected child’s spine in October 2017. The surgeons trained for the surgery on a 3D printed model of the patient, and were able to perfect the timing of the surgery as a result.
The researchers’ findings are detailed in their paper titled “An investigation into the effect of changing the computed tomography slice reconstruction interval on the spatial replication accuracy of three‐dimensional printed anatomical models constructed by fused deposition modelling” published in the Journal of Medical Radiation Sciences on February 13th 2020. The study was co-authored by Ben Searle and Deborah Starkey.
You can now nominate for the 2020 3D Printing Industry Awards. Cast your vote to help decide this year’s winners.
To stay up to date with the latest 3D printing news, don’t forget to subscribe to the 3D Printing Industry newsletter or follow us on Twitter or liking our page on Facebook.
Looking for a job in the additive manufacturing industry? Visit 3D Printing Jobs for a selection of roles in the industry.
Featured image shows the Malyan M200 3D printer used to produce the researchers’ test models. Image via Malyan 3D.



