The risk, when writing about 3D bioprinting is that the “over-simplification” that is necessary to convey the news article’s message in the title gives an over-hyped idea of what has been achieved, with the inevitable let down that follows when we focus in on the actual facts. So, the recent video published by Popular Mechanics, which shows human heart cells made from skin cells (which were first transformed into plenipotentiary stem cells), assembled together through a 3D bioprinting process and beating autonomously is a fascinating step forward and, yet, it is only a tiny part of the incredible work on tissue engineering carried out by Dr. Anthony Atala, Director of the Wake Forest Institute for Regenerative Medicine, that holds amazing possibilities for the future and even for the present.
The beating heart cells, which can be considered a miniature 3D printed heart in and of themselves, form what are now being defined as “tissue organoids” (that is, “modules” of tissue cells that can be assembled into more complex shapes through a bioprinter). The heart organoid represents the meeting point between Atala’s current work on tissue engineering – which led him to implant functioning bladders, a urethra, and even a vagina into human patients – and his Defense-funded work on the body-on-a-chip program, a next generation, 3D printed drug testing device which was well described in this Live Science article from 2013.
The US Space and Naval Warfare Systems Center is funding this program with $24 million as part of a larger effort by the U.S. Defense Threat Reduction Agency. “Miniature lab-engineered organ-like hearts, lungs, livers, and blood vessels – linked together with a circulating blood substitute – will be used both to predict the effects of chemical and biologic agents and to test the effectiveness of potential treatments,” Atala said to Popular Mechanics.
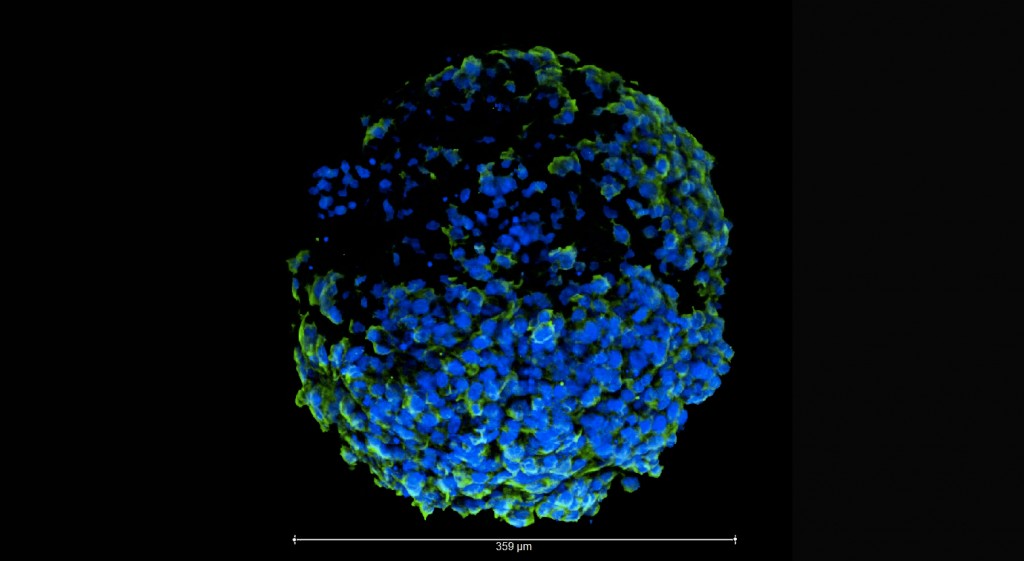
In this specific case, the environmental cues were a special medium to keep them at the same temperature as the human body. The scientists also stimulated the miniature organ with electrical or chemical cues to alter the beating patterns. Growing them in three-dimensions through a 3D bioprinting systems allows them to interact with each other more easily, as they would in the human body. Although this project does not aim for the full reproduction of a human heart for implantation, it may help scientists find new ways to “assemble” human organs, without the use of a 3D printed polymer-based scaffold. Instead, they might find ways to even let complex organs self-assemble. In that case, we may have functional 3D printed organs even sooner than we think and the title of this article would, perhaps, turn out to to be an understatement in the end.


