An academic team from the University of the West of England’s Center for Fine Print Research (CFPR) is using 3D printing to produce realistic organs for use in surgical training.
According to the researchers, the aim of the project is to create model organs that mimic the “appearance, elasticity and consistency” of human tissue. By creating organ simulators that look and feel real, surgical training becomes more representative of real life and can ultimately aid in lessening patient risk.
Dr. James Clark, General Surgeon at Royal Cornwall Hospital and Co-supervisor of the project, explains how surgical simulators have become an essential part of surgical education in modern times. He points out that complex surgical operations often require “good quality reproducible models which enable the trainee to get a true realistic feel for the operation”.
The three-year project is funded by the Appearance Printing European Advanced Research School (ApPEARS) at the Norwegian University of Science and Technology (NTNU).
The 3D printing of low cost, high fidelity medical models
Led by David Huson, Senior Research Fellow at CFPR, the work is an extension of former pilot studies, building on how 3D printing can develop low cost, high fidelity medical products. Huson describes it as “a cross-disciplinary project” as it combines scientists, artists, and surgeons to develop and test a working prototype. An advantage of using organ simulators, he explains, is that they offer a more ethical alternative to human cadavers or animal subjects “which are often expensive to obtain and difficult to access”.
Marine Shao, an Associate at CFPR, points out that this project will be different from the already existing commercial organ simulators, which “tend to reproduce just the most common procedures and do not accurately replicate the properties and feel of human tissue”. Due to its relative cost-efficiency, the UWE simulator can be produced anywhere and is much more accessible. Shao explains that one of the main aims is to tackle the limitations present in current organ simulators. By doing so, a cheaper and more realistic product can be developed.

Which organs were replicated?
Huson’s team set out to create a prototype capable of facilitating a laparoscopic bile duct exploration – a complex surgical procedure used to remove stones lodged in the bile duct. To do this, they replicated the interconnected tissues and inner structures of multiple organs including the duodenum, gallbladder, liver, pancreas, and bile duct.
Unlike pre-existing models on the market, typically made from silicon, these organ simulators were made up of a combination of undisclosed materials. By combining 3D printing with traditional casting methods, the team was able to combine these materials together, the result being a product that is representative of the complex human gastrointestinal system.
In addition to the geometries of the gastrointestinal organs, the researchers also replicated the acoustic properties of the soft tissue. Since the laparoscopic bile duct procedure involves using ultrasound to examine the bile duct for stones, effectuate anatomical delineation and detect anomalies. It is, therefore, a fundamental trait that the organ simulators replicate acoustic properties of soft tissue, as this enables surgeons to perform realistic ultrasound examinations in a monitored environment.
3D printing in healthcare research
There is evidence that, at an educational level, training with organ simulators has been proven effective. In a recent literature review concerning 3D printing in urology, medical students were asked to accurately locate tumors, first with exclusively MRI and then with the help of 3D printed prostate models. With MRI, there was a 47% difference between the success rates of students and experts whilst with 3D printing, this plunged to 17%.
Another prospect comes from work by UC Davis Health, where surgeons are using both 3D printed anatomical models and life-like organs. Combining the latter with “a high-resolution 3D model of the injury” allowed the surgeons to increase their precision as they had access to the exact measurements of their patients. Equally, researchers at Tampere University have also found 3D printed models, specifically of nasal channels, to be a promising and lower-cost method of improving nasal surgery. The extensive research in the field indicates the potentiality that organ simulators have in ameliorating surgical operations as well as medical advancements.
The 4th annual 3D Printing Industry Awards are coming up in November 2020 and we need a trophy. To be in with a chance of winning a brand new Craftbot Flow IDEX XL 3D printer, enter the MyMiniFactory trophy design competition here. We’re happy to accept submissions until the 30th of September 2020.
Subscribe to the 3D Printing Industry newsletter for the latest news in additive manufacturing. You can also stay connected by following us on Twitter and liking us on Facebook.
Looking for a career in additive manufacturing? Visit 3D Printing Jobs for a selection of roles in the industry.
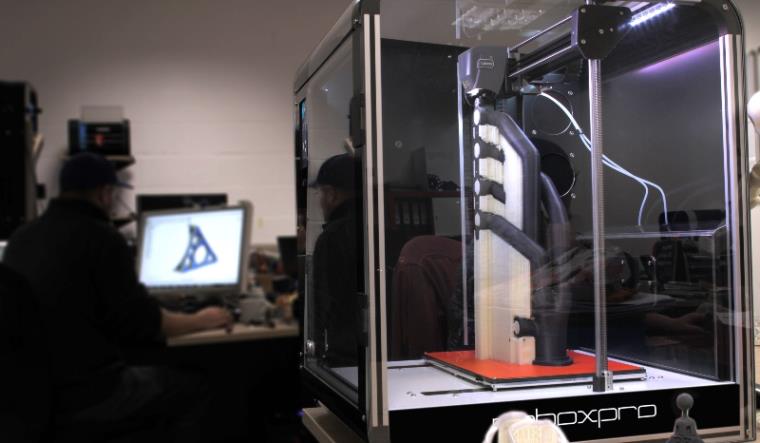
Featured image shows Life-like physical model for simulated medical training. Image via CFPR.


