A team of researchers from Tampere University, Finland, has experimented with a new method of nasal surgery preparation using 3D printing. With the aim of determining whether or not 3D printing could realistically replicate the anatomy of a nasal cavity and the airflow through it, the team took to scanning and printing a set of internal nasal channels. Extensive analysis of the prints has shown that perhaps the technology could be used as a faster, lower-cost method of rhinomanometry evaluation.
Surgical planning
The modeling and printing of various limbs and organs have previously been used by medical professionals when planning out a high-risk operation. Using these models in the crucial pre-surgery stage can help increase the success rate of the procedure as it aids with visualization. Alternatively, 3D printed models can also be used in the classroom as a teaching tool for budding medical students.
According to the researchers, however, 3D printing has not yet been used for the modeling of internal nasal channels. They attribute this to the relative complexity of the nose, making it difficult to maintain precision which is key when examining something as sensitive as airflow. Instead, 3D models of the nose tend to be traditionally cast in silicone, with particle image velocimetry (PIV) and computational fluid dynamics (CFD) used as technical analysis tools. Unfortunately, producing and analyzing these models is a slow, laborious, and often costly process – one which 3D printing hopes to replace.
3D printed nasal channels
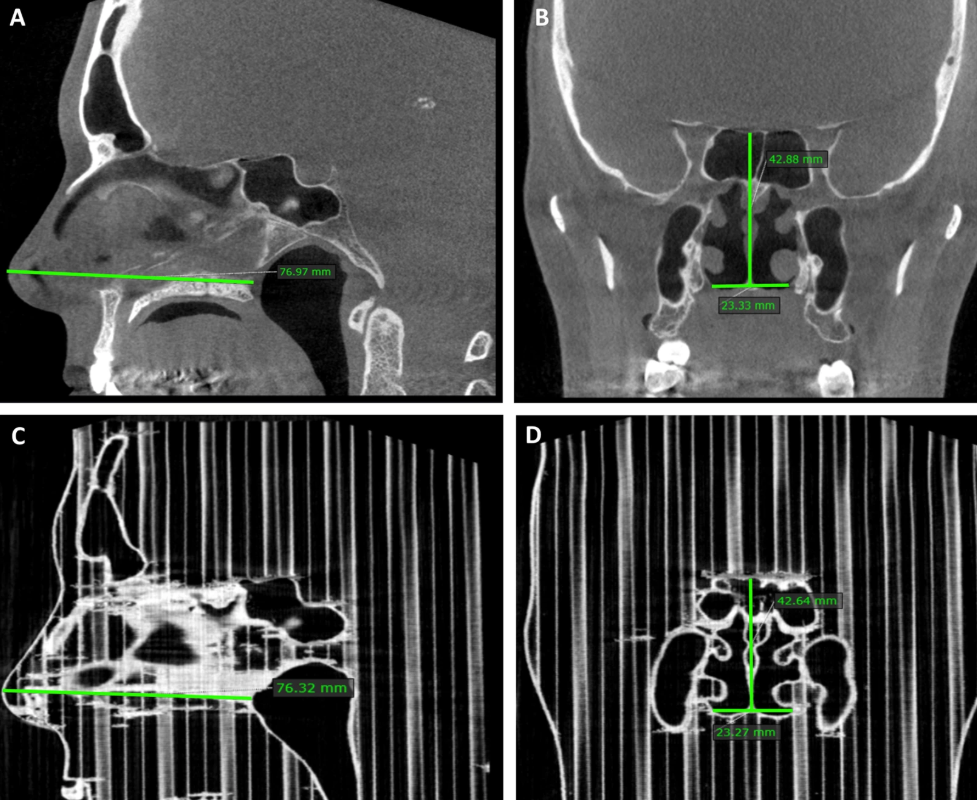
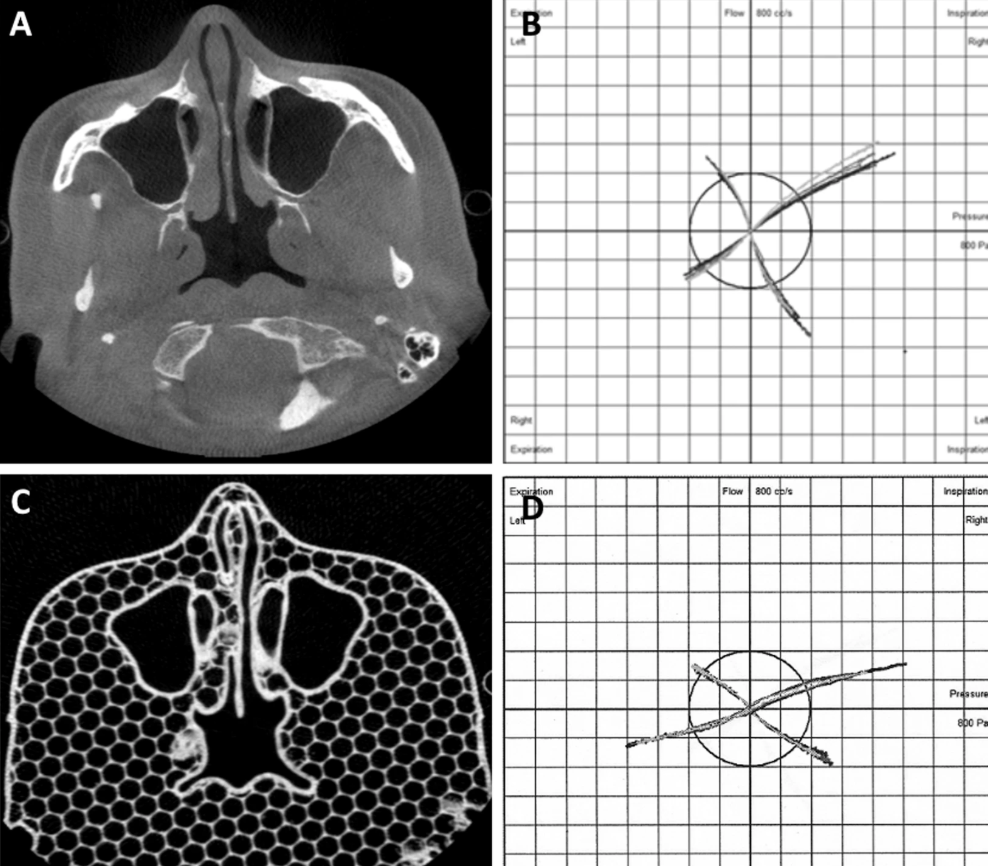
The team started off by taking the cone-beam computed tomography (CBCT) scans of five adult patients with chronic nasal congestion. CBCT was chosen due to its relatively low dose of radiation when compared to conventional CT scans. The scan data was converted into a 3D printable format using MATLAB, which was then prepared and sliced using Slic3r. To maintain dimensional precision where possible, supports were omitted and all printing was done on a Lulzbot Taz 4 3D printer with PLA.
In order to then accurately compare the prints to the noses of the patients, CBCT scans of all the PLA parts were taken. Looking at the maxillary sinus volumes of the two scan groups, the 3D printed parts were slightly off by about 1.05 cubic millimeters, although this was considered to be very close to the actual value range.
Finally, the airflow resistance of the printed parts was compared to the airflow resistance of the patient’s noses. This was done using an instrument called a rhinomanometer – a device built specifically for the purpose. Using it on the patients was straightforward but the printed parts required some DIY ingenuity, so the researchers connected tubes to the back of the prints and stuck the other end up their own noses for science. With similar resistance values in both groups, the team concluded that their previously unseen method of 3D printing nasal channels showed great promise for clinical use.
Further details of the study can be found in the paper titled ‘Three-Dimensional Printing of the Nasal Cavities for Clinical Experiments’. It is co-authored by Olli Valtonen, Jaakko Ormiskangas, Ilkka Kivekäs, Ville Rantanen, Marc Dean, Dennis Poe, Jorma Järnstedt, Jukka Lekkala, Pentti Saarenrinne, and Markus Rautiainen.
The 3D printing of medical models extends beyond academia. Digital manufacturing service provider Fast Radius and Axial3D, a UK-based medical technology firm, have recently announced a new ‘DICOM-to-print’ service aimed at surgeons and hospitals across North America. The duo plans to improve surgical planning by supplying micron-accurate, patient-specific anatomical models.
Elsewhere, in Queensland, researchers have released a study that challenges the suitability of FDM for producing anatomical reconstructions. The team claims that inaccuracies and defects in the replicas can potentially cause harm to patients through suboptimal treatment planning, and would like to optimize the process through their work.
Subscribe to the 3D Printing Industry newsletter for the latest news in additive manufacturing. You can also stay connected by following us on Twitter and liking us on Facebook.
Looking for a career in additive manufacturing? Visit 3D Printing Jobs for a selection of roles in the industry.
Featured image shows measurements of a patient and the corresponding PLA model. Image via Tampere University.


