According to the German Organ Transplantation Foundation (DSO), the number of organ donors in the first half of 2013 has declined more than 18% year on year, mainly because of recent organ transplant scandals. 3D bio printing offers an alternative to dependence upon donation. Let’s look at bio printing and a new 10,523,108.60 € project that aims to further the progress of 3D bio printing tissues in this emerging science that promises organs on demand.
Critical illnesses can already be successfully treated today by replacing cells, tissue or organs. Government, industry and the research establishment have therefore been working hard to improve methods and procedures for artificially producing tissue.
To summarise the relevance of 3D printing for general readers as this is an depth article:
• Branched vessel structures with dimensions from > 100 µm will be generated by Inkjet printing technology.
• High-resolution laser processes like stereolithography and multiphoton polymerisaton are used for smaller vessels and pores.
• The surrounding network for cell cultivation will be generated by electro spinning.
Scientists of the Fraunhofer Institute for Interfacial Engineering and Biotechnology (IGB) in Stuttgart have succeeded in developing suitable bio-inks for this printing technology. The transparent liquids consist of components from the natural tissue matrix and living cells.
The substance is based on a well-known biological material: gelatin. Gelatin is derived from collagen, the main constituent of native tissue. The researchers have chemically modified the gelling behaviour of the gelatin to adapt the biological molecules for printing.
Instead of gelling like unmodified gelatin, the bio-inks remain fluid during printing. Only after they are irradiated with UV light are they crosslinked and cured to form hydrogels. These are polymers containing a huge amount of water like native tissue but remain stable in aqueous environments and when being warmed up to a physiological temperature of 37°C.
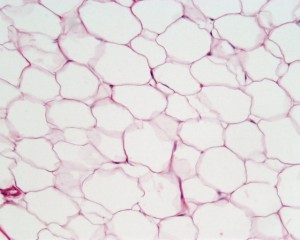
The researchers can control the chemical modification of the biological molecules so that the resulting gels have differing strengths and swelling characteristics enabling imitation of the properties of natural tissue — from solid cartilage to soft adipose tissue.
Dr. Kirsten Borchers described the approach: “We are concentrating at the moment on the ‘natural’ variant. That way we remain very close to the original material. Even if the potential for synthetic hydrogels is big, we still need to learn a fair amount about the interactions between the artificial substances and cells or natural tissue. Our biomolecule-based variants provide the cells with a natural environment instead, and therefore can promote the self-organising behaviour of the printed cells to form a functional tissue model.”
The printers at the labs in Stuttgart have a lot in common with conventional office printers: the ink reservoirs and jets are all the same. The differences are discovered only under close inspection. For example, the heater on the ink container with which the right temperature of the bio-inks is set. The number of jets and tanks is smaller than in the office counterpart as well.
“We would like to increase the number of these in cooperation with industry and other Fraunhofer Institutes in order to simultaneously print using various inks with different cells and matrices. This way we can come closer to replicating complex structures and different types of tissue,” says Borchers.
The big challenge at the moment is to produce vascularised tissue. This means tissue that has its own system of blood vessels through which the tissue can be provided with nutrients. IGB is working on this jointly with other partners under Project ArtiVasc 3D – ‘Artificial vascularised scaffolds for 3D-tissue regeneration.’
ArtiVasc 3D will provide a micro- and nano-scale based manufacturing and functionalisation technology for the generation of fully vascularised bioartificial fatty tissue. The artificial vascularisation will, for the first time, allow a connection to the natural tissue enabling entire nutrition and metabolism. By combining the fatty tissue with a dermal and epidermal cell layer a 3-layered skin equivalent will be developed.
ArtiVasc 3D builds on the innovative combination of micro-scale printing, nano-scale multiphoton polymerisation electro-spinning, chemical and morphological surface modification and cell culture. In a multidisciplinary approach, experts in biomaterial development, cell-matrix interaction, angiogenesis, tissue engineering, simulation and fabrication methods work together on generating standardised vascularised soft tissue in a fully automated and standardised manufacturing approach.
This vascularised tissue will be applied as a bioartificial tissue in reconstruction surgery, for example for burned skin or after tumour resection in breast cancer surgery. Also, the new artificial vascularised skin will be used as innovative in vitro skin equivalent for pharmaceutical, cosmetics or chemical substance testing, which promises to be an approach to reducing testing upon animals.
“This step is very important for printing tissue or entire organs in the future. Only once we are successful in producing tissue that can be nourished through a system of blood vessels can printing larger tissue structures become feasible,” said Dr. Kirsten Borchers in closing.
Other recent bio-printing developments include the use of vitamin B2, as covered here.