The nominations for the 2021 3D Printing Industry Awards are now open. Who do you think should make the shortlists for this year’s show? Have your say now.
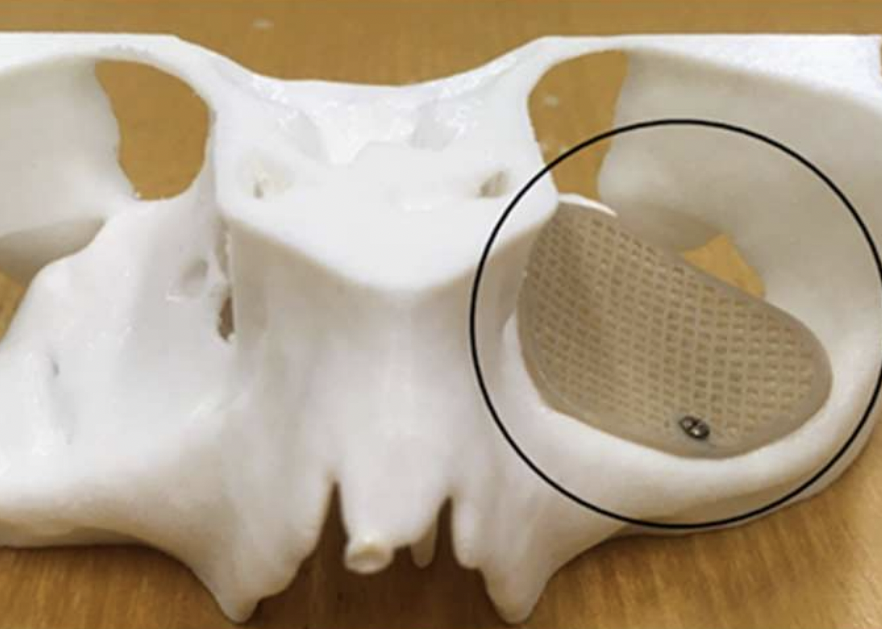
Researchers at the University of Basel have developed a novel 3D printed implant for treating eye socket fractures that carries a reduced risk of patient rejection.
Constructed using a Prusa i3 3D printer and PEEK filament, the team’s grafts are able to overcome the bioinertness of their material thanks to their porous features, which can be tailored to enhance cellular repair. Through Finite Element (FE) analysis, the team have also found their devices to be highly-customizable, meaning that in future, they could be adapted to meet the needs of individual optical patients.
“The printing of high-temperature, implantable-grade thermoplastic polymers such as PEEK, paves the way for a more sophisticated generation of biomaterials,” said the team in their paper. “Implementing FDM [3D printing] at point-of-care offers less material wastage, easy operator training, faster implant production, increased cost-effectiveness and patient specificity.”
Treating ‘orbital floor fractures’
When it comes to facial wounds, so-called ‘orbital floor fractures’ represent one of the most gruesome injuries possible. A common side-effect of being hit by a blunt force to the face, orbital floor fractures effectively see the wall under affected patients’ eyes become damaged, and the ailment can be very difficult to treat given the site’s obscured location.
Although advances in Virtual Surgical Planning (VSP) continue to make addressing such eye socket fractures easier than ever before, related surgical materials remain a roadblock to optimal patient outcomes. PEEK, meanwhile, is a robust 3D printing polymer in its own right, and has shown considerable potential in this area, but according to the Swiss team its lack of bioactivity is a cause for “clinical concern.”
In the past, researchers have toyed with the idea of coating PEEK to improve its osseointegration, but poor binding can lead to the material’s degradation and ultimately osteolysis. Alternatively, given the technology’s inherent design flexibility, 3D printing is increasingly finding surgical graft applications, in which it allows for the realization of porous implants that foster greater cell regrowth.
However, despite the clinical potential of additive manufactured medical devices, the Basel researchers found no existing studies that examine the behaviors of PEEK FDM 3D printed implants, thus they’ve now established a workflow which enables the production of customized grafts, that feature improved surgical applicability.
Striving for PEEK performance
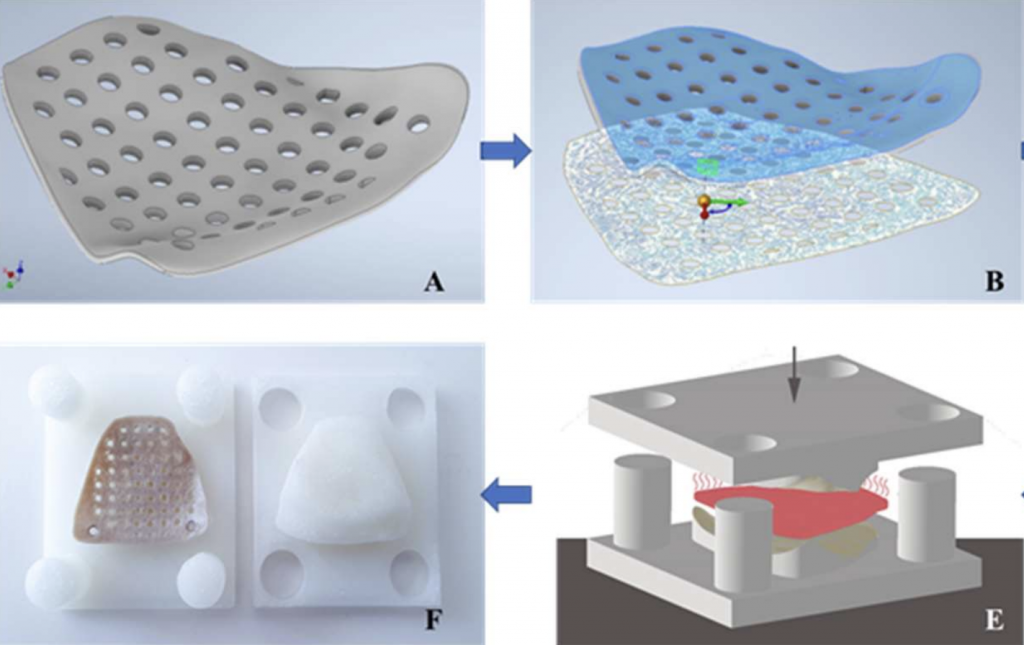
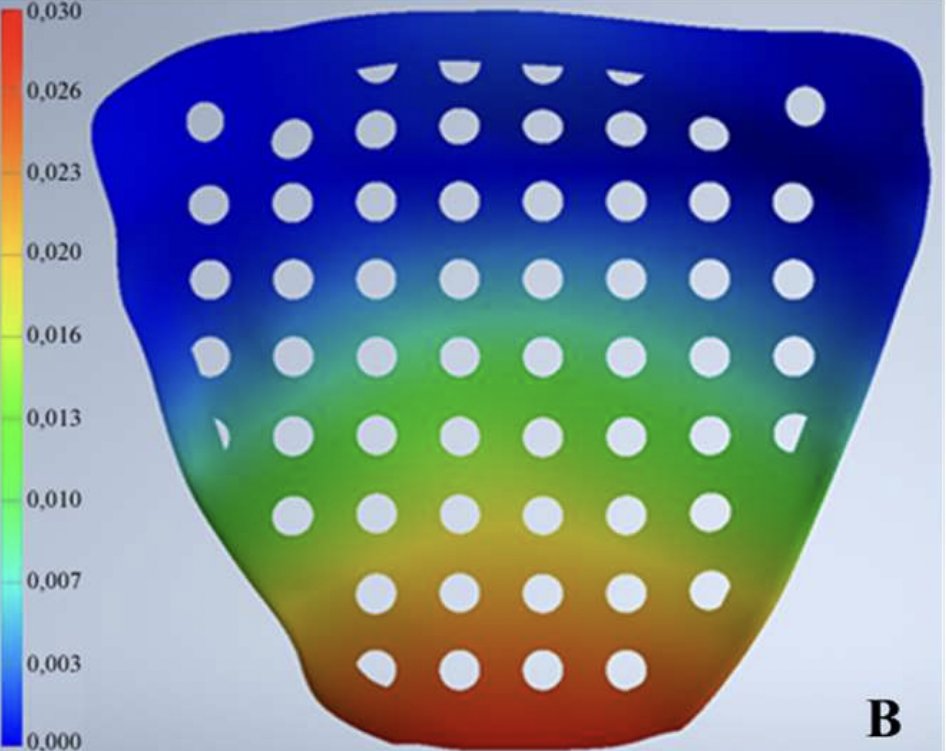
To begin with, the team created FE models of several different orbital mesh implant designs, and used simulation software to test their performance against clinical ‘worst case scenarios.’ Based on their findings, the researchers opted to integrate 1.5 mm screw points into each of their devices’ ‘rims’ as a means of holding them in place during end-use, before exporting them as STL files for printing.
Interestingly, the team’s initial models failed due to their complex overhangs, forcing the researchers to adopt a ‘reverse-origami’ approach. In practise, this meant digitally converting their 3D implants into 2D ones using the ‘unwrap’ function in Autodesk’s Inventor program, before extruding them flat and manually removing them from the print bed.
In order to make their grafts 3D again, the researchers then used a mold and press box to heat and compress them back into their desired form, before grading and analyzing their qualities. Each device was marked based on their deformation under 0.3N as well as their morphological fit, and unsurprisingly, results showed that the thinnest implants also exhibited the highest levels of stress under pressure.
With regards to fit and accuracy compared to patient models, each of the devices scored a minimum of ‘satisfactory’ by the team’s own scale, while rectangularly-shaped implants were marked as the most robust. The team therefore concluded their approach to be as important as the resulting devices, and that FE modelling had allowed them to rapidly iterate towards a patient-friendly design.
“Using Multi-criteria decision-making (MCDM) [assessments], FE-based computational analysis and FDM can be evaluated in multiple treatment options,” explained the team in their paper. “This approach demonstrates that a range of combinations can be assessed to reach the most effective clinical solution.”
3D printing’s optical potential
Given the enclosed nature of the human eye socket, it can be a very difficult area to operate on, but surgeons are increasingly finding that 3D printing and modelling can help optimize their patients’ chances. Earlier this year, for instance, doctors at the Israeli Galilee Medical Center (GMC) combined 3D printing with VR, to develop a novel way of treating optical fractures.
In the past, researchers at the University of Porto have deployed additive manufacturing in a similar way, to help reconstruct the eye of a 47-year-old woman. Working with the Institute of Science and Innovation in Mechanical and Industrial Engineering, the team were able to create a high-quality prosthetic, while reducing its associated lead time and costs.
Elsewhere, at the Brazilian Paulista University, scientists have developed a means of capturing and 3D printing facial prosthetics for those living with maxillofacial defects. Based on smartphone-captured scans, the team have already been able to create prostheses for a cancer survivor who lost her right eye and part of her jaw.
The researchers’ findings are detailed in their paper titled “A multi-criteria assessment strategy for 3D printed porous Polyetheretherketone (PEEK) patient-specific implants for orbital wall reconstruction.”
The study was co-authored by Neha Sharma, Dennis Welker, Soheila Aghlmandi, Michaela Maintz, Hans-Florian Zeilhofer, Philipp Honigmann, Thomas Seifert and Florian M. Thieringer.
The nominations for the 2021 3D Printing Industry Awards are now open. Who do you think should make the shortlists for this year’s show? Have your say now.
To stay up to date with the latest 3D printing news, don’t forget to subscribe to the 3D Printing Industry newsletter or follow us on Twitter or liking our page on Facebook.
For a deeper-dive into additive manufacturing, you can now subscribe to our Youtube channel, featuring discussion, de-briefs and shots of 3D printing in-action.
Are you looking for a job in the additive manufacturing industry? Visit 3D Printing Jobs for a selection of roles in the industry.
Featured image shows the researchers’ 3D printed eye socket implant installed on a skull model. Photo via the University of Basel.


