A team of researchers from Texas A&M University’s Department of Biomedical Engineering has designed and 3D bioprinted a highly realistic model of a blood vessel.
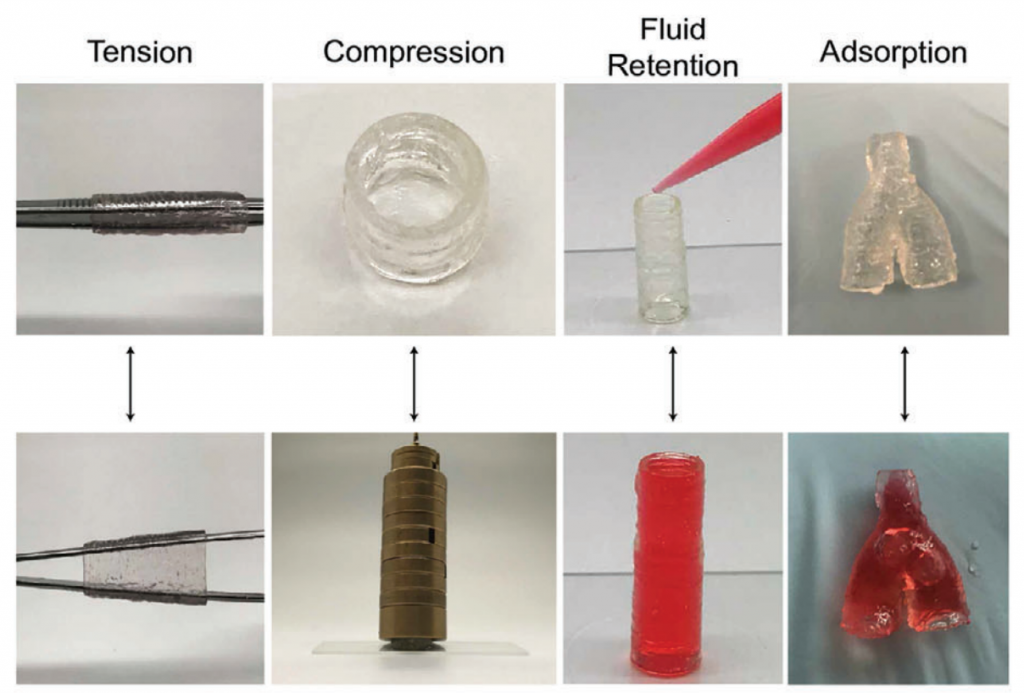
The model is made of a newly nanoengineered, purpose-built hydrogel bioink and closely mimics the natural vascular function of a real blood vessel, as well as its disease response. The team hopes its work can pave the way for advanced cardiovascular drug development, expediting treatment approval while eliminating the need for animal and human testing altogether.
“A remarkably unique characteristic of this nanoengineered bioink is that regardless of cell density, it demonstrates a high printability and ability to protect encapsulated cells against high shear forces in the bioprinting process,” said Akhilesh Gaharwar, associate professor at the university and co-author of the study. “Remarkably, 3D bioprinted cells maintain a healthy phenotype and remain viable for nearly one month post-fabrication.”
3D bioprinting and vascular diseases
According to the research team, blood vessel diseases such as aneurysms, peripheral artery disease, and blood clots account for around 31% of deaths worldwide. Despite the harrowing figure, advancements in cardiovascular drugs have reportedly slowed down over the past two decades.
This can be attributed to the challenge of transforming experimental treatments into approved ones, which largely stems from the discrepancies between in vitro studies and in vivo studies. Quite simply, we need more lab models that actually respond like the vessels in our bodies – this is where 3D bioprinting can lend a hand.
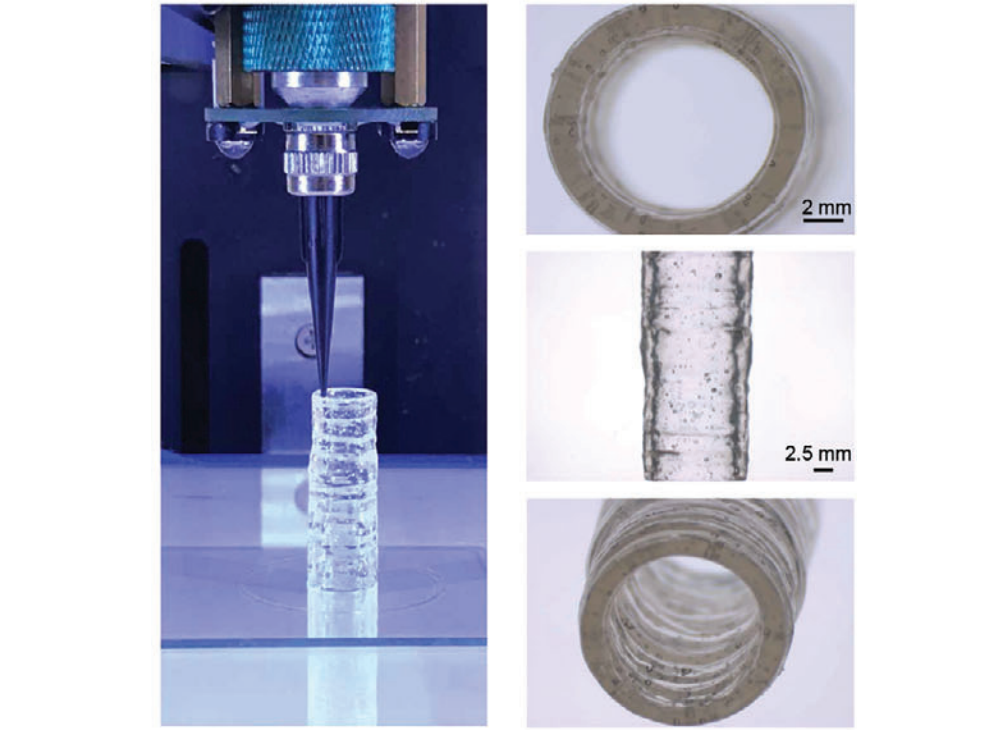
With bioprinting, tissue structures can be embedded with real living cells and manufactured in a layer-by-layer manner. This makes it possible to design models with much greater precision, allowing them to better mimic the native structures of blood vessels. Unfortunately, the bioink materials required to enable this are largely limited in terms of printability and their capacity to deposit high densities of living cells, rendering many of them ineffective in clinical settings.

Testing for disease and drug impact
In a bid to overcome the limitations of readily available bioinks, Gaharwar and his team developed their own. The new material is specially designed for anatomically accurate, multicellular blood vessels, offering an improved resolution for both the macro-structure of the vessel and the microstructure of the tissue.
Gaharwar writes, “Here, a new class of nanoengineered hydrogel-based cell-laden bioinks is introduced, that can be printed into 3D blood vessels to recapitulate both the physical and chemical microenvironments of native human vasculature.”
The bioink comprises cultures of endothelial cells as well as vascular smooth muscle cells: the building blocks required to accurately test for disease impact and the effects of drugs. It’s also characterized by its excellent printability and has even been shown to protect the embedded living cells from the forces of the extrusion-based printing process. The hopes are that the 3D bioprinted blood vessel model can one day be used to better understand vascular disease pathophysiology and assess the efficacy of therapeutics and toxins in preclinical trials.
Further details of the study can be found in the paper titled ‘3D Bioprinted Multicellular Vascular Models’. It is co-authored by Akhilesh Gaharwar, Abhishek Jain, et al.
Blood vessels aren’t the only tissues being bioprinted for drug development applications. Earlier this summer, volumetric 3D bioprinter manufacturer Readily3D used additive manufacturing to develop a miniature 3D printed living model of the human pancreas. Designed to facilitate diabetes medicine testing, the stem cell-containing biological tissue can be printed in just 30 seconds.
Elsewhere, South Korean pharmaceutical company HK inno.N recently announced plans to use artificial 3D printed skin to test new autoimmune and skin disorder drugs. The 3D printed flesh is set to be used to conduct in-depth research into the effectiveness of different skin disease medications. If successful, the tissues could be used to replace animal testing, which is known to be an ongoing issue in the cosmetics industry.
Subscribe to the 3D Printing Industry newsletter for the latest news in additive manufacturing. You can also stay connected by following us on Twitter, liking us on Facebook, and tuning into the 3D Printing Industry YouTube Channel.
Looking for a career in additive manufacturing? Visit 3D Printing Jobs for a selection of roles in the industry.
Featured image shows Karli Gold ’20, a former biomedical engineering doctoral student who worked with Akhilesh Gaharwar on his 3D bioprinted models. Photo via TAMU.


