An international group of scientists led by the University of Adelaide and the University of Stuttgart has used 3D microprinting to develop an Optical Coherence Tomography (OCT) endoscope.
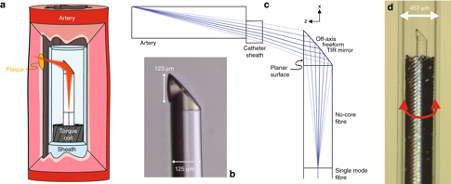
The research team’s novel probe fabrication technique uses side-facing freeform micro-optics (less than 130 µm in diameter) to 3D print directly onto single-mode fibers. Measuring just 0.48mm, the resulting microscopic imaging device is small enough to enter blood vessels and overcomes the resolution issues encountered by existing technologies. The improved 3D images provided by the enhanced endoscope’s camera could enable doctors to better understand the causes of cardiac disease, potentially allowing them to prevent heart attacks before they happen.
“Until now, we couldn’t make high-quality endoscopes this small,” said Dr. Simon Thiele, Group Leader, Optical Design, and Simulation at the University of Stuttgart. “Using 3D micro printing, we are able to print complicated lenses that are too small to see with the naked eye. The entire endoscope, with a protective plastic casing, is less than half a millimeter across.”
“It’s exciting to work on a project where we take these innovations and build them into something so useful. It’s amazing what we can do when we put engineers and medical clinicians together.”
3D printing, endoscopes, and vascular health
For medical staff, fiber-optic endoscopes have quickly become an essential clinical tool for providing real-time guidance during a medical intervention. OCT endoscopies, in particular, have been utilized in a large number of surgical cases, providing assistance in an estimated 410,000 operations to date within Australia alone.
Nonetheless, despite its widespread applications, endoscopic technology hasn’t been perfected yet. Miniaturized high-resolution probes remain in high-demand, not only to enable the imaging of delicate, narrow luminal organs but also to minimize the discomfort of probe insertion within veterinary operations. Often, animals such as mice are also used as models for human diseases, and in order to make the most of such experimentation, a more versatile solution is required.
Previous studies have also found that conventional probes aren’t able to capture images of any structures deeper than 100 μm, limiting their potentially life-saving applications within cardiac care. “A major factor in heart disease is the plaques, made up of fats, cholesterol, and other substances that build up in the vessel walls,” explained Jiawen Li, Co-author, and Lecturer at the University of Adelaide.
“Preclinical and clinical diagnostics increasingly rely on visualizing the structure of the blood vessels to better understand the disease. Miniaturized endoscopes, which act like tiny cameras, allow doctors to see how these plaques form and explore new ways to treat them.”
According to the researchers, current probe manufacturing techniques are also inadequate, as endoscopes often suffer from spherical aberration, low resolution, or a shallow depth of focus. What’s more, while resolution and depth of focus are often traded off in existing probes, within miniaturized devices, their physical apertures are very small, and no appropriate compromise exists. Additionally, in OCT imaging, intravascular probes are deployed within a transparent catheter sheath, to protect the patient from trauma during the camera’s rotation.
Optically, the cable cover causes astigmatism to the camera, leading it to lose focus, and current manufacturing methods have no means of mitigating this. While previous approaches have focused on splicing existing fiber lenses, these have also failed to gain the same level of resolution as conventional OCT imaging. In order to overcome these limitations, the research team set about using two-photon polymerization to 3D print 125-μm diameter micro-optics directly onto a single-fiber compound.
Creating and testing the 3D printed endoscope
In order to manufacture their additive endoscope, the researchers spliced a 450 μm length of no-core fiber into a 20 cm length of single-mode fiber, which expanded the light beam before it reached the micro-optic camera. The beam shaping micro-optic was then 3D printed directly onto the distal end of the material, using a Nanoscribe two-photon lithography system.
The researchers’ production method was found to compensate for astigmatism caused by the mandatory transparent catheter sheath. Moreover, the fiber assembly was fixed inside a thin-wall torque coil, which allowed the device to be maneuvered precisely to the opposite end of the imaging probe.
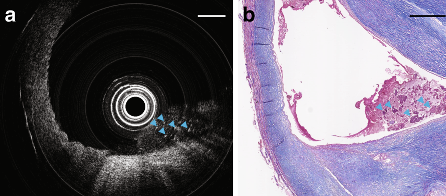
To evaluate the performance of their ultra-thin OCT probe for scanning tissue samples, the research team attempted to capture images inside a freshly removed human carotid artery. Although the blocked blood vessel exhibited severe stenosis, the team’s ultra-thin probe was still able to move effortlessly through it and then be pulled back. In addition, the endoscopic camera was able to detect a necrotic core of dead cells, a critical feature for identifying high-risk plaques that can cause heart attacks.
Further OCT imaging tests were carried out in situ on a mouse’s thoracic aorta. The probe was able to capture imaging without any obvious rotational distortion, and 3D imaging was successfully performed within very small arteries, with the tiniest being less than 0.5mm. Pictures also showed thick densely packed adipocytes, which had a diameter of 15–25 μm, indicating that the 3D printed probe could identify microstructural features via in situ imaging.
As a result, the researchers considered their experiments to be sufficient proof that their printed OCT device was an improvement on currently-used endoscopes. According to the team, the success of their 3D printed approach could lead to its adoption within a range of clinical applications.
“Apart from the value of using imaging probes in small animals, this ultra-thin aberration-corrected probe can also allow safe access to delicate but difficult-to-reach organs, enable a high-resolution cross-sectional imaging capability, and potentially lead to enhanced patient safety and improved health outcomes,” stated the research team in their paper.
Using additive innovation to combat heart disease
While the German/Australian research team’s approach is novel, many other research groups have also used 3D printing to combat heart disease, albeit often in the shape of polymer heart models.
The University of Kentucky (UK) College of Medicine, for instance, is 3D printing custom heart models to aid physicians and their patients. Costing just $5, the replicas are being produced as an accurate, pre-surgical tool to enable the precise fitting of heart-assisting implants.
Researchers from Stanford University’s School of Medicine, on the other hand, are developing 3D printed cardiac catheter surgical devices. The product can be used by surgeons to map a heart’s electrical activity, ultimately detecting rhythm disturbances in a patient’s heartbeats.
Great Ormond Street Hospital (GOSH) is using 3D printed replicas of children’s hearts to enable surgeons to better plan complex and crucial heart surgeries. The 3D printed models could lead to quicker, more effective surgeries and faster recoveries for patients.
The researchers’ findings are detailed in their paper titled “Ultrathin monolithic 3D printed optical coherence tomography endoscopy for preclinical and clinical use,” which was published in the Light: Science and Applications journal. The report was co-authored by Jiawen Li, Simon Thiele, Bryden C. Quirk, Rodney W. Kirk, Johan W. Verjans, Emma Akers, Christina A. Bursill, Stephen J. Nicholls, Alois M. Herkommer, Harald Giessen and Robert A. McLaughlin.
You can now nominate for the 2020 3D Printing Industry Awards. Cast your vote to help decide this year’s winners.
To stay up to date with the latest 3D printing news, don’t forget to subscribe to the 3D Printing Industry newsletter or follow us on Twitter or liking our page on Facebook.
Looking for a job in the additive manufacturing industry? Visit 3D Printing Jobs for a selection of roles in the industry.
Featured image shows the research team’s 3D printed endoscope. Image via Simon Thiele and Jiawen Li.


